Atrial Fibrillation (AFib)
Atrial fibrillation (AFib) is an irregular heart rhythm that begins in your heart’s upper chambers (atria). Symptoms include fatigue, heart palpitations, trouble breathing and dizziness. Risk factors include high blood pressure, coronary artery disease and having obesity. Medications and procedures (like ablation) can lower your risk of a stroke.
What Is AFib?
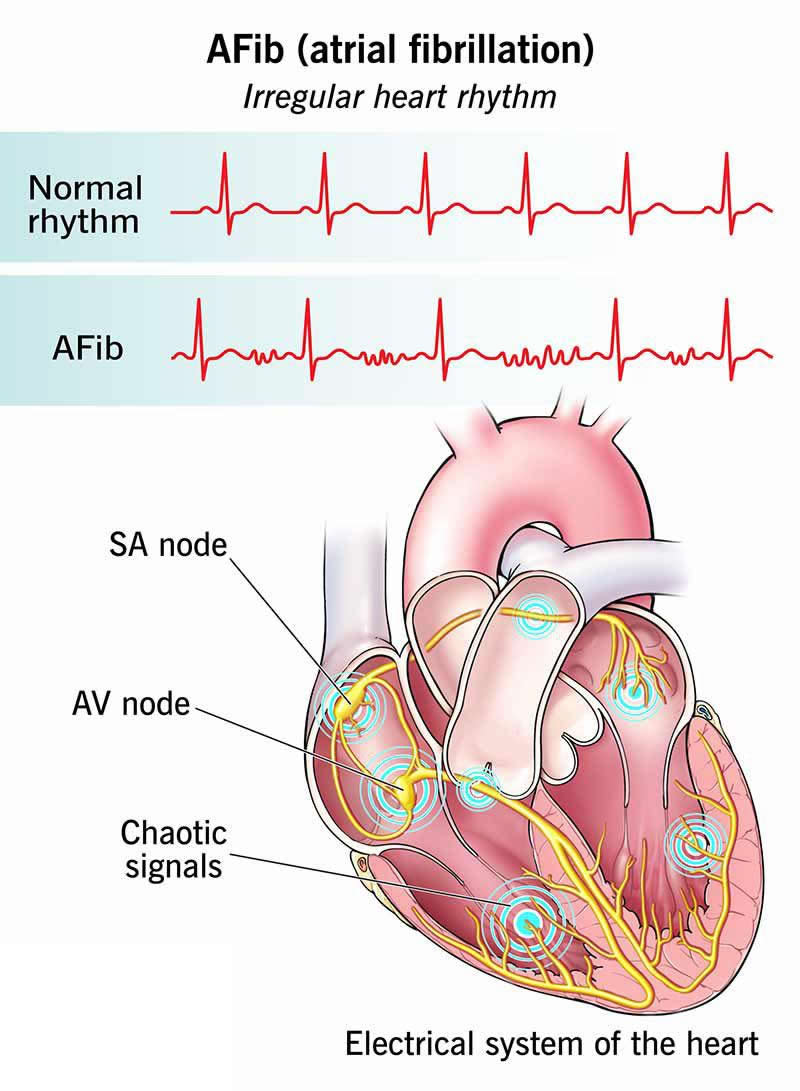
AFib (atrial fibrillation) is an irregular heart rhythm that begins in the upper chambers of your heart. With AFib, your heart’s electrical system doesn’t work as it should. Instead of sending electrical signals in a steady pattern, it sends many different signals at the same time.
This causes a fast, chaotic rhythm in your upper chambers (atria). As a result, your atria can’t do a good job of contracting or pumping blood into your lower chambers (ventricles). Your ventricles, which respond to your atria, also contract irregularly, causing a fast, irregular heartbeat. The heartbeat that you feel comes from your ventricles’ contractions.
You can think of Afib like several conductors directing an orchestra instead of just one. The musicians wouldn’t know who to follow or what to do. The music would lose its rhythm.
Atrial fibrillation can lead to serious complications like a stroke or heart failure. That’s why it’s important to learn the symptoms and talk with your healthcare provider about your personal risk factors.
Symptoms and Causes
Symptoms of atrial fibrillation
AFib symptoms include:
- A feeling of butterflies or a fish flopping in your chest, or the sensation that your heart is racing or pounding (heart palpitations)
- Extreme fatigue
- Dizziness or lightheadedness
- Fainting (syncope)
- Shortness of breath (dyspnea)
- Chest pain (angina)
How serious is being in AFib?
Whether or not you feel symptoms, being in AFib is serious. It means your heart is out of rhythm. When your heart isn’t beating normally, you have a higher risk of dangerous blood clots forming in your heart and traveling to vital organs such as your brain, resulting in a stroke, as well as other complications. If you have symptoms of AFib, contact your healthcare provider right away.
Call 911 or your local emergency number if you:
- Have chest pain
- Have severe shortness of breath
- Faint or feel like you might faint
AFib causes
Changes to your heart’s tissue and electrical system cause atrial fibrillation. Here’s what can cause such changes:
- Other forms of cardiovascular disease. These include coronary artery disease, valve disease and heart failure.
- Other medical conditions. These include high blood pressure, overweight, obesity, hyperthyroidism, chronic kidney disease and obstructive sleep apnea.
- Genetic variants. Certain gene changes are associated with AFib, according to the latest research. These genetic links may explain some cases of AFib that begin at a younger age.
- Heart surgery. It’s possible for AFib to begin after heart surgery you have for another reason. AFib can also happen when you’re recovering from non-cardiac surgery.
Risk factors
Having any of the medical conditions listed above raises your risk for AFib. Other risk factors include:
- Increasing age. Your risk for AFib goes up as you get older, and especially after age 65.
- Excessive alcohol use. Drinking more than the recommended limit, including “binge drinking,” raises your risk for AFib. Researchers are still studying the risks of staying at or below the limit.
- Critical illness. Serious illnesses that require hospitalization (like sepsis or severe COVID-19) raise your risk of developing AFib.
- Lack of physical activity. You’re more likely to develop AFib if you don’t get enough movement each day.
- Extreme exercise training. Physical activity helps your heart, but it’s possible to have too much of a good thing. You’re more likely to develop AFib if you do extreme exercise or high-intensity endurance training for at least three hours a day over many years.
Diagnosis and Tests
How doctors diagnose this condition
An electrocardiogram (ECG/EKG) diagnoses atrial fibrillation. This test creates a graph of the electrical signals traveling through your heart. The results can show if you have AFib or other types of arrhythmias.
Your provider will also:
- Do a physical exam and review your medical history
- Order blood tests to check for other conditions, including those that could affect your AFib treatment plan
- Order an echocardiogram (echo) to evaluate your heart’s structure and function
- Possibly ask you to wear a monitor (Holter monitor or cardiac event monitor) to record your heart’s electrical activity during your daily activities
AFib stages
AFib is a progressive condition. That means it develops in stages and can get worse over time. Here are the updated stages that healthcare providers use when diagnosing and treating AFib:
- Stage 1: At risk for AFib
- Stage 2: Pre-AFib
- Stage 3: AFib
- Stage 4: Permanent AFib
At risk for AFib
You have certain risk factors for AFib, including:
- High blood pressure
- Obesity
- Diabetes
- Sleep apnea
- Excessive alcohol use
- Poor cardiovascular endurance
- Age over 65
Pre-AFib
You have changes to your heart’s electrical activity or structure that further raise your risk for AFib. Signs providers look for include:
- Atrial tachycardia
- Atrial flutter
- Enlarged left and/or right atrium
- Frequent ectopic heartbeats
You’re also at stage 2 if you have certain conditions linked with a high risk for AFib. These include:
- Coronary artery disease
- Heart failure
- Heart valve disease
- Hyperthyroidism
- Hypertrophic cardiomyopathy
- Neuromuscular disorders
AFib
An ECG/EKG shows you have atrial fibrillation. But this can mean a lot of different things. You might have symptoms that come and go on their own. Or you might have AFib episodes that persist despite treatment. Symptoms might go away after treatment, but return down the road.
That’s why healthcare providers divide this stage into four substages.
- Paroxysmal AFib. Episodes happen every now and then. Each episode lasts less than one week and usually stops on its own without treatment. You might still feel unwell during these short episodes. And you have a higher risk of stroke than those who don’t have AFib.
- Persistent AFib. Episodes are continuous, meaning they keep coming back. Each episode lasts more than one week. You need treatment to stop an episode.
- Long-standing persistent AFib. Episodes are continuous for one year or longer.
- Successful AFib ablation. AFib stops after a surgery or a catheter-based procedure.
Once you’re diagnosed with AFib, you might transition among any of these substages. For example, persistent AFib might return some time after a successful ablation.
Permanent AFib
This means you’re no longer trying to manage AFib with treatments and you’re constantly in AFib. You and your healthcare provider make this decision together based on your situation.
Management and Treatment
How is AFib treated?
Atrial fibrillation treatment involves one or more of the following:
- Lifestyle changes
- Medications
- Ablation therapy
- Other procedures
Lifestyle changes
These are things you can do from day to day to help keep AFib from progressing. Lifestyle changes are important across all the stages of AFib — including before you have any symptoms. Your provider will help you:
- Reach and maintain a weight that’s healthy for you
- Limit alcohol consumption
- Avoid tobacco use
- Get the recommended amount of physical activity
- Manage any conditions that raise your risk for AFib, including high blood pressure, obesity, obstructive sleep apnea and diabetes
Medication
Your provider may prescribe medications to control your heart rate and/or heart rhythm. These medications can prevent damage to your heart and help reduce symptoms that make you feel uncomfortable or anxious. Your provider may also prescribe medications that lower your risk of blood clots that could lead to a stroke.
The medications you need to manage AFib may change over time. In general, you’ll need to take blood thinners (anticoagulants) if you’re at risk of having a stroke. Providers typically prescribe oral anticoagulants (DOACs) like:
- Apixaban
- Rivaroxaban
- Dabigatran
- Edoxaban
In some cases, providers prescribe warfarin instead of a DOAC.
Medications to manage your heart rate include:
Medications that help your heart beat in a normal (sinus) rhythm include:
Ablation for AFib
Ablation for AFib is an umbrella term for a group of procedures that create scar tissue in your heart. We often think of scars as harmful, but in this case, the scar tissue helps your heart’s electrical system work better. The scars block the abnormal electrical signals to help your heart beat in a normal rhythm.
Specific procedures your cardiologist might recommend for AFib include:
- Catheter ablation. This is a minimally invasive procedure. Your surgeon guides thin tubes through your blood vessels to your heart. Pulmonary vein isolation (PVI) ablation is a specific type of catheter ablation that providers commonly use to treat AFib.
- Maze procedure. This is also called surgical ablation. Your surgeon creates scar tissue that follows a maze pattern to block abnormal signals. Surgical ablation usually takes place during heart surgery done for another reason (like CABG or valve surgery).
Other procedures
Other procedures that treat AFib include:
- Cardioversion. Your provider uses a device (defibrillator) or medicine to get your heart rhythm back to normal.
- Left atrial appendage (LAA) closure. If you can’t tolerate blood thinners, you might qualify for implantation of a device to lower your risk of a stroke (left atrial appendage occlusion device). This procedure seals off a sac in your heart where blood clots can easily form.
Outlook / Prognosis
Can your heart go back to normal after AFib?
Yes. Sometimes, your heart will go back to a normal rhythm on its own. This is the case with paroxysmal AFib. If you have persistent or long-standing AFib, you need treatment to end an episode.
But it’s important to know there’s no cure for AFib. Once you have it, you have it for life. Your provider will help you manage the condition. Treatment can lower your risk of a stroke and help you experience fewer symptoms.
What is the average life expectancy with AFib?
A study published in 2024 found that people with AFib had a shorter life expectancy than those without AFib. The number of years lost from their life expectancy varied by their age at diagnosis. The younger you are at diagnosis, the shorter your life expectancy, and the more years you lose compared to others your age without AFib.
| Age at diagnosis | Average life expectancy |
|---|---|
| 30 years old | 72 years (about 11.3 years shorter than expected) |
| 50 years old | 75 years (about 9.2 years shorter than expected) |
| 70 years old | 82 years (about 5.4 years shorter than expected) |
| Age at diagnosis | |
| 30 years old | |
| Average life expectancy | |
| 72 years (about 11.3 years shorter than expected) | |
| 50 years old | |
| Average life expectancy | |
| 75 years (about 9.2 years shorter than expected) | |
| 70 years old | |
| Average life expectancy | |
| 82 years (about 5.4 years shorter than expected) |
Remember that statistics just tell part of the story. Working closely with your healthcare team to manage AFib and any other medical conditions can give you the best chance at a long life.
Living With
How do I take care of myself?
The same habits that lower your risk of Afib help you feel better when you have it. Eating nutritious foods and getting 30 minutes of physical activity five days a week helps your heart. You can break up your activity into 10-minute chunks to make it easier. Cutting out tobacco products and alcohol is good for your heart, too.
When should I see my healthcare provider?
There’s no single schedule to follow. It all depends on your symptoms and treatment plan, and whether you need follow-ups after a procedure. So, it’s important to talk with your provider and make a plan together. Make sure you go to all your scheduled appointments. Keep track of the medications you’re taking and bring a list of your medications to every visit. It’s also a good idea to keep the list in your wallet so it’s with you in emergencies.
At each visit, be sure to share any new symptoms or problems you’re having, like side effects from medication. Be sure to ask your provider before taking over-the-counter (OTC) medicines, like those for cold and flu, and nutritional supplements. Sometimes, these products can affect your heart rate or interact with your prescription medications.
What questions should I ask my healthcare provider?
Questions to consider asking your provider may include:
- How can I reduce my risk factors?
- Can you connect me with a dietitian?
- Can you recommend any local health and fitness programs?
Additional Common Questions
How can I check for Afib at home?
If you think you have Afib symptoms, it’s important to call your healthcare provider right away to discuss how you’re feeling. Your provider may ask you to check your pulse. If it feels erratic or weak, that could be a sign you’re in Afib.
But sometimes, you might not notice any changes in your pulse, especially if your Afib isn’t advanced. You may instead just feel tired or out of breath. You may not know if your symptoms are from Afib or something else. That’s why a call to your provider is essential. You can’t diagnose Afib yourself.
How common is Afib?
More than 33 million people age 55+ worldwide have an Afib diagnosis. Estimates predict that 12 million people in the U.S. will have Afib by 2030. Afib causes nearly half a million hospitalizations a year in the U.S. and leads to more and more deaths with each passing year.
A note from Wockr
An AFib diagnosis can feel scary, confusing or overwhelming. But you’re not alone. You’re one of the millions of people learning new strategies for managing AFib while still enjoying life. Your healthcare provider can tell you more about treatment options, resources and support communities.