Borderline Personality Disorder vs. Bipolar Disorder
BPD is associated with more frequent mood swings and difficult relationships, while bipolar disorder has more persistent, long-lasting depressive and manic episodes

Borderline personality disorder (BPD) and bipolar disorder share many symptoms, like mood swings and impulsive behavior. But they’re actually different conditions. BPD is a personality disorder, while bipolar disorder is a mood disorder.
Psychiatrist Edward Kilbane, MD, explains why these two are often confused with each other.
BPD vs. bipolar disorder
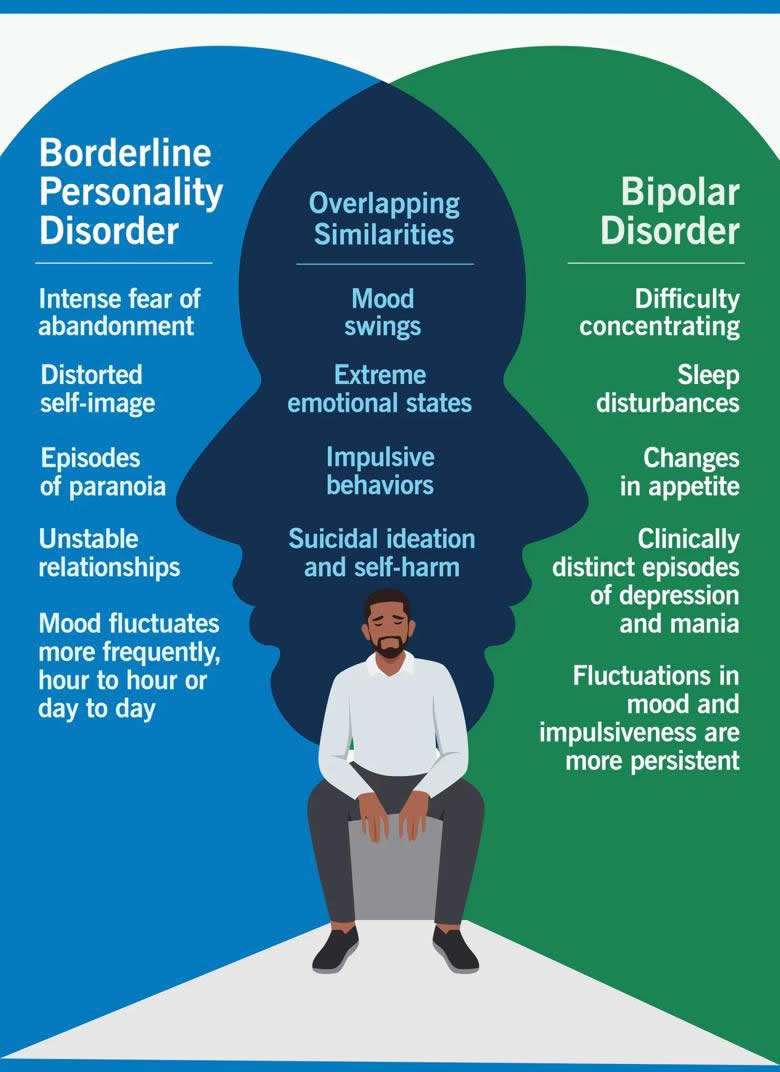
Borderline personality disorder is distinct from bipolar disorder.
In BPD, mood and behavior change rapidly in response to significant stress, especially when interacting with other people. BPD affects many parts of a person’s life. It involves using unhealthy coping habits that go against social norms, leading to a range of mental health symptoms.
“BPD is called ‘borderline’ because it involves mood, anxiety and psychotic symptoms,” explains Dr. Kilbane. “With bipolar disorder, mood symptoms of depression or mania take longer to develop. They’re more sustained and less reactive to social stressors.”
People with bipolar disorder can also have significant changes in:
- Sleep
- Speech
- Energy
- Activity
“The primary difference here is that a mood disorder involves either depression or mania or some combination of the two,” he continues. “A personality disorder involves an unhealthy pattern of coping. It usually develops early in life before the age of 18, and it’s not really in line with how the rest of society copes or interacts with each other.”
Everyone experiences these conditions differently. The severity of their symptoms also depends on several factors. We don’t know the exact causes of BPD or bipolar disorder, but possible risk factors include:
- Genetic risks and family history of BPD or bipolar disorder
- Early environmental stress, like child abuse or trauma
- Changes in brain structure, size or function
BPD
Borderline personality disorder involves deep-seated character traits that affect your relationships and the way you see yourself and others. It’s characterized by:
- Difficulty managing emotions
- Impulsivity
- Unstable relationships with yourself and others
These feelings and traits can become so ingrained in someone’s identity that they tend to impact their behaviors, thoughts and views of others.
“They can get micro-psychotic episodes where they’re stressed out and are not in touch with reality, but those tend to resolve quite quickly,” says Dr. Kilbane.
Symptoms
“With BPD, mood symptoms change drastically within the same day or from hour to hour. One day, everything can be fine, and the next day, everything can be awful,” illustrates Dr. Kilbane. “It’s different from bipolar disorder, where depression and mania persist.”
Other symptoms of BPD include:
- Frequent, intense mood swings
- Unstable relationships
- Feeling empty
- Fear of being abandoned
- Bouts of intense anger
- Episodes of paranoia or brief difficulty understanding what’s real and what’s not
- Distorted self-image involving feelings of shame, guilt or emptiness
- Impulsive, dangerous behaviors, like reckless driving or substance misuse
- Ongoing thoughts of suicide and harming yourself on purpose
Treatment
Treatment for BPD often combines medications with therapy.
Mentalization-based therapy teaches people with BPD how to step into other people’s shoes. The focus is on better understanding how others feel so they can respond to them appropriately.
Dialectical behavior therapy (DBT), on the other hand, teaches you how to process and regulate your own emotions so you can develop a better emotional response. This teaches you how to sit with uncomfortable feelings without immediately acting on them.
In practice, someone with BPD might meet one-on-one with a therapist weekly. They’ll also have DBT in a group therapy setting where people share what they’re feeling and process those emotions together.
“When people engage in these types of therapy, they can have more meaningful, stable relationships in the long term. They also have fewer feelings of emptiness and less chronic suicidality,” notes Dr. Kilbane. “With therapy, people with BPD can really get on top of these symptoms and lead meaningful lives.”
Bipolar disorder
Bipolar disorder is a mood disorder that causes extreme shifts between depression and mania. During depressive episodes, you tend to have feelings of:
- Hopelessness
- Extreme fatigue
- Lack of motivation
During mania, your emotions are elevated and more extreme, giving way to:
- Irritability
- Hyperactivity
- Increased energy
Bipolar II disorder also involves manic episodes (called hypomania), but they don’t last as long or disrupt daily life.
“With bipolar disorder, the majority of mood episodes are depressive. And that’s why a lot of people with bipolar might be diagnosed with major depressive disorder first,” says Dr. Kilbane.
Symptoms
With bipolar disorder, moods tend to last days to weeks (not hours, as with BPD). Symptoms are often triggered by significant stress or changes in sleep patterns. They include depressive symptoms like:
- No interest in activities you used to enjoy (anhedonia)
- Crying a lot
- Trouble focusing
- Changes in appetite
- Sleep issues
- Thoughts or attempts of suicide
Manic symptoms include:
- Frequent, intense mood swings
- Decreased need for sleep
- Elevated, euphoric or irritable mood
- Racing thoughts
- Impulsive behaviors
- Excessive energy and motor activity
- Paranoia or hallucinations
“The impulsiveness you see in borderline personality disorder can look very similar to the impulsiveness in bipolar disorder. But impulsivity is quite brief with BPD,” clarifies Dr. Kilbane. “In bipolar, impulsivity is something that persists day to day. And unless it’s treated, it can persist for quite some time.”
Treatment
Similar to BPD, bipolar disorder treatment involves a combination of medication and therapy, but with more emphasis on medications to stabilize mood.
“Medications tend to work better for bipolar disorder because we think that it’s more of an issue with chemicals in your brain compared to borderline personality disorder,” shares Dr. Kilbane. “If we can help stabilize your mood, then the therapy side of treatment becomes more effective.”
Is one worse than the other?
Both BPD and bipolar disorder come with unique sets of challenges. One isn’t worse than the other. They’re both lifelong mental health conditions that require medication and therapy. It’s also possible to be diagnosed with both BPD and bipolar disorder. In those instances, it can be even more difficult to treat because the conditions can aggravate each other.
“If you have borderline personality disorder and you think you’re not good enough and nobody cares about you, then you might think there’s no point in taking medications or going to therapy,” notes Dr. Kilbane. “When you stop taking medication and you start to get depressed or manic because of bipolar disorder, then things can quickly spiral.”
If you recognize any of the signs or symptoms of BPD or bipolar disorder, make an appointment with your primary care provider or a behavioral health specialist. They’ll be able to verify your diagnosis, answer any questions you have and get you the help you need.