Burning Mouth Syndrome
Burning mouth syndrome is a painful condition that affects your tongue, lips and other areas inside your mouth. Anyone can get it, but it’s most common in postmenopausal people. There’s no cure, but treatment can help you manage painful symptoms.
Overview
What is burning mouth syndrome?
Burning mouth syndrome (BMS) is when your tongue, roof of your mouth or lips feel like they’re burning. It can also occur anywhere else in your mouth or throat. BMS can happen fast, and you might not know why. It might feel like something really hot (like coffee) burned your tongue. The medical term for burning mouth syndrome is “glossodynia” (pronounced “glaa-sow-DI-nee-uh”).
If you have BMS, the burning feeling might get worse as the day goes on. Your mouth might feel fine when you first wake up, but then start to burn later. When you go to sleep, the pain might fade. But then, when you wake up, it starts all over again.
Along with the burning feeling, your mouth might taste bitter or metallic. Some people have the sensation of dry mouth even though they have enough saliva. The burning can get so bad that it causes people to feel depressed or anxious.
It’s frustrating to have pain and not know why. Treatment can’t cure burning mouth syndrome, but it can help manage your symptoms. And learning more about possible triggers can help reduce the frequency of flare-ups.
Types of burning mouth syndrome
There are two types of burning mouth syndrome:
- Primary BMS is when your mouth feels like it’s burning, but there’s no clear reason why.
- Secondary BMS is when your mouth burns because of another condition. If you fix that condition, the burning mouth sensation usually goes away, too.
Who is most at risk for burning mouth syndrome?
Burning mouth is most common in postmenopausal people over 60. That’s because lower estrogen levels cause decreased taste bud sensitivity.
Your genetic ability to taste also plays a role. You might be a:
- Nontasterwho doesn’t taste things very strongly
- Medium tasterwho tastes things the way most other people do
- Supertaster, who tastes things really strongly
A lot of people with burning mouth syndrome are supertasters who don’t taste things as strongly as they used to. Research shows that many people with BMS also grind their teeth. This can make the burning feeling worse.
Symptoms and Causes
What are the symptoms of burning mouth syndrome?
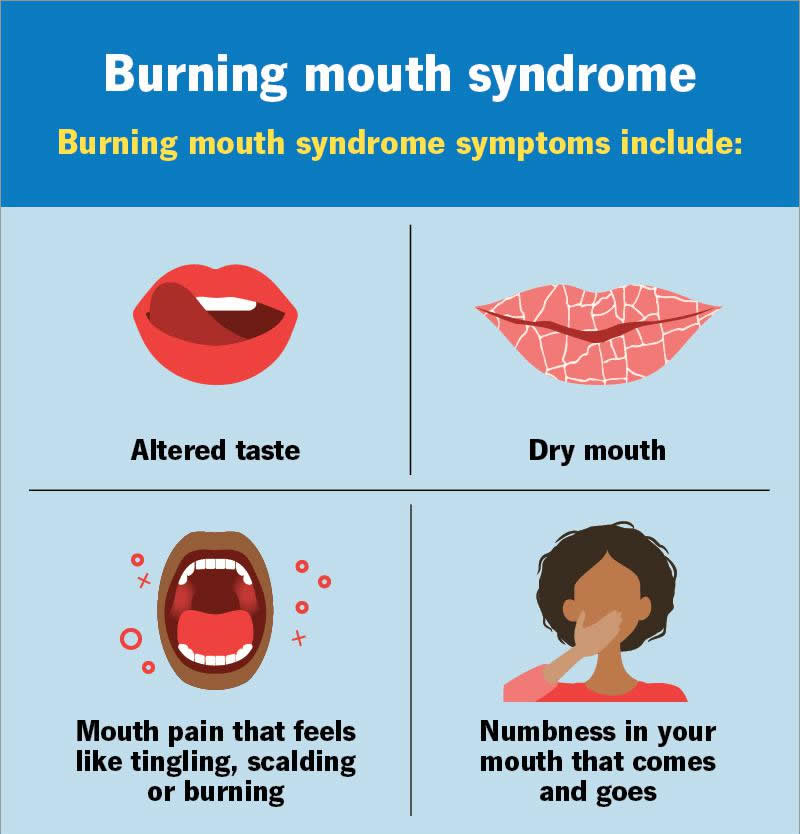
Burning mouth syndrome symptoms include:
- Altered taste
- Dry mouth
- Mouth pain that feels like tingling, scalding or burning
- Numbness in your mouth that comes and goes
Burning mouth syndrome doesn’t cause visible symptoms like bumps or discoloration.
What causes burning mouth syndrome?
Researchers believe the cause of primary BMS is nerve damage affecting the area of your tongue that controls taste and pain. This makes your mouth feel like it’s burning and changes how things taste to you. Researchers think the nerve damage comes from factors like stress, certain medications, nutritional deficiencies or underlying medical conditions.
Medical conditions that can cause secondary BMS include:
- Acid reflux
- Allergies to certain foods or dental products
- Dry mouth
- Hormonal changes
- Nerve damage
- Oral infections like thrush
- Stress
- Teeth grinding or jaw clenching
Risk factors
You’re more likely to develop burning mouth syndrome if you:
- Are in postmenopause
- Have certain health conditions like diabetes or Sjögren’s syndrome
- Have chronic anxiety and/or depression
- Have geographic tongue
- Have nutritional deficiencies (a lack of iron, zinc or vitamins B6 and B12, for example)
- Take certain medications prescribed for depression or high blood pressure
- Are female
Diagnosis and Tests
How is burning mouth syndrome diagnosed?
If you have symptoms, see a dentist first. They can start with a visual exam and refer you to a specialist if needed. A healthcare provider will need to run tests to rule out other conditions. Possible tests include:
- Allergy test
- Blood test
- Imaging tests like dental X-rays, CT scans or MRI
- Oral swab test
- Saliva test
- Tissue biopsy
Management and Treatment
How is burning mouth syndrome treated?
These burning mouth syndrome remedies may help ease general discomfort:
- Mouth rinses with mild numbing effects
- Pain relievers like acetaminophen (Tylenol®) or ibuprofen (Advil®)
- Saliva substitutes like Biotene®
- Some antidepressant and antiseizure medications
The U.S. Food and Drug Administration (FDA) hasn’t approved any drugs specifically for BMS. But the medications mentioned may help manage your symptoms. Sometimes, it can take a while to find the medication that works best. Your healthcare provider can help.
If your healthcare provider knows what’s causing burning mouth syndrome, treating that cause can help. For example, if you grind your teeth, your dentist can make you a custom mouth guard for you to wear. If menopause triggers BMS, hormone replacement therapy may help.
Identifying the root cause isn’t always possible. But when it is, it may help find treatment quicker.
How can I get instant relief from burning mouth syndrome?
You may be able to ease burning mouth pain by doing the following:
- Chew sugar-free gum. (This encourages saliva production.)
- Drink cold water.
- Sip on cold beverages throughout the day.
- Suck on ice chips.
These actions won’t get rid of burning mouth syndrome. But they can help reduce pain during flare-ups.
Outlook / Prognosis
Will burning mouth syndrome ever go away?
Without treatment, burning mouth syndrome can last for months or even years. That can be a long time to live with mouth pain. BMS treatment can provide relief within days or weeks. Talk to your healthcare provider about your specific treatment and when you can expect to feel better.
Prevention
Can burning mouth syndrome be prevented?
You can’t prevent BMS. But you can reduce your risk for flare-ups by avoiding anything that irritates your mouth, including:
- Beverages containing alcohol
- Extremely hot foods or beverages
- High-acidic foods or drinks (like citrus juices)
- Hot and spicy foods or drinks
- Mouthwash containing alcohol
- Smoking or vaping
Also, make sure you’re getting enough vitamin B12, folate and iron.
Living With
When should I see my healthcare provider?
Schedule an appointment with a healthcare provider if the burning in your mouth:
- Comes with additional symptoms like swelling or blisters
- Gets worse
- Lasts longer than a few days
- Occurs for no apparent reason
What questions should I ask my doctor?
Here are some questions you might want to ask your healthcare provider if you have burning mouth syndrome:
- Do you know what might have caused this flare-up?
- What tests will I need?
- What kind of treatment do you recommend?
- How long should I try one treatment before trying another?
A note from Wockr
When your mouth feels like it’s on fire, it can be hard to think about anything else. Burning mouth syndrome (BMS) is frustrating — and it can take a while to find a remedy that works. Treatment can’t get rid of the condition for good, but it can help with pain and other symptoms. If you think you might have burning mouth syndrome, talk to a dentist first. They can help.