Castleman Disease
Castleman disease refers to a group of rare conditions that cause swelling and tissue changes in your lymph nodes. The two primary types are unicentric Castleman disease and multicentric Castleman disease. Symptoms, treatment options and prognosis vary depending on the type.
What Is Castleman Disease?
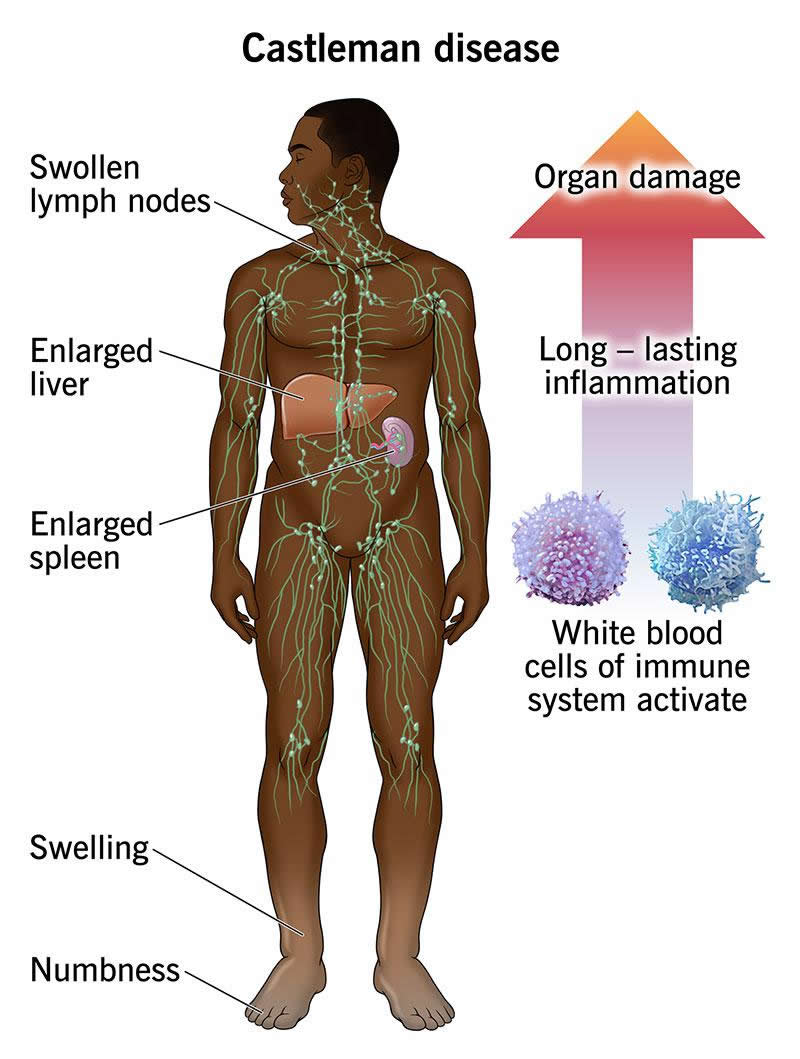
Castleman disease is a group of disorders that involve a hyperactive immune system. Typically, healthy immune systems activate to fight germs invading your body. Then, they settle down once the threat is gone. But if you have Castleman disease, your immune system remains activated. This leads to long-lasting inflammation that can damage organs.
Meanwhile, your lymph nodes work overtime to filter germs and the immune cells that fight them. This causes an overgrowth of cells that leads to swollen lymph nodes. The lymph nodes don’t just get bigger. Castleman disease causes changes in the tissue of affected lymph nodes.
Castleman disease is rare. There are only about 4,300 to 5,200 new Castleman disease cases diagnosed in the U.S. each year. There’s still a lot that doctors are learning about this condition. In the meantime, treatment involves customizing the right therapies based on your unique diagnosis.
Types of Castleman disease
There are two main types of Castleman disease.
Unicentric Castleman disease (UCD)
Unicentric Castleman disease (UCD) causes enlargement of one or more lymph nodes in one region of your body. About 3 in 4 cases of Castleman disease are UCD.
Multicentric Castleman disease (MCD)
Multicentric Castleman disease (MCD) causes lymph node enlargement in many regions of your body. Healthcare providers classify MCD as:
- POEMS-associated MCD. POEMS is a rare blood disorder that sometimes accompanies MCD.
- HHV-8-associated MCD. This type of MCD happens alongside human herpes virus-8 (HHV-8) infection. You’re more likely to have this type if you’re HIV positive or immunocompromised.
- Idiopathic MCD (iMCD). The most common form of MCD is idiopathic. “Idiopathic” means that its causes are unknown.
There are three subtypes of iMCD:
- iMCD associated with TAFRO. TAFRO syndrome sometimes accompanies iMCD. TAFRO gets its name from its associated signs and symptoms. They are thrombocytopenia (low platelets), anasarca (swelling from fluid build-up), fever, renal (kidney) dysfunction and organomegaly (enlarged spleen or liver).
- iMCD with idiopathic plasmacytic lymphadenopathy (iMCD-IPL). MCD-IPL may cause high platelets. With this subtype, your white blood cells may make too many antibodies.
- iMCD, not otherwise specified (iMCD-NOS). iMCD-NOS has unknown causes and isn’t associated with TAFRO.
Symptoms and Causes
Symptoms of Castleman disease
Castleman disease symptoms vary depending on the type. You likely won’t have symptoms with unicentric Castleman disease. Enlarged lymph nodes may be the only sign. Sometimes, symptoms occur when an enlarged lymph node creates pressure on a nearby organ.
MCD is more likely to cause noticeable symptoms. In addition to enlarged lymph nodes, signs and symptoms include:
- Fever
- Fatigue (may be a sign of anemia)
- Night sweats
- Nausea and vomiting
- Unexplained weight loss
- Swelling in your feet, ankles or abdomen
- Enlarged spleen (splenomegaly) or liver (hepatomegaly)
- Numbness in your hands and feet (peripheral neuropathy)
Castleman disease causes
While the causes of unicentric Castleman disease (UCD) are unknown, an HHV-8 infection is associated with multicentric Castleman disease (MCD).
Scientists are researching potential causes of UCD and iMCD. These include infections other than HHV-8, gene mutations and autoimmune responses.
Risk factors
There aren’t any known risk factors for UCD or iMCD. You’re at increased risk of developing HHV-8-associated MCD if you have HIV or another condition that weakens your immune system.
People of any age can develop Castleman disease, but most people diagnosed are ages of 30 to 60.
Complications of Castleman disease
Castleman disease increases your chances of developing cancer, including lymphoma.
Although it’s rare, people with UCD are at risk of developing a serious condition called paraneoplastic pemphigus (PNP). MCD can increase your risk of developing infections that can damage organs. The damage can be life-threatening without treatment.
Your healthcare provider will monitor your condition to prevent complications whenever possible.
Diagnosis and Tests
How doctors diagnose Castleman disease
Castleman disease symptoms are similar to those in other conditions, including common illnesses like the flu. Your healthcare provider may rule out these conditions first. Then, they’ll perform tests to diagnose Castleman disease and determine the type.
Tests and procedures may include:
- Lab tests. Your provider will check for abnormal blood cell counts and other microscopic signs of Castleman disease. They may perform an HIV test. A positive result is typical with HHV-8-associated MCD.
- Imaging tests. CT scans and PET scans allow your provider to locate enlarged lymph nodes in your body. They may check for other signs of Castleman disease, like an enlarged liver or spleen.
- Lymph node biopsy. A biopsy is the only way to confirm that you have Castleman disease. Your provider will examine lymph node tissue beneath a microscope to check for signs of the disease.
Management and Treatment
How is Castleman disease managed or treated?
Treatment for Castleman disease varies according to the type.
Unicentric Castleman disease (UCD) treatment
Surgery to remove the affected lymph nodes is the primary treatment for UCD. You may need radiation therapy or immunotherapy before surgery. These therapies shrink the growths on your lymph nodes, making them easier to remove.
If surgeons can’t remove the affected lymph node and you don’t have symptoms, your provider may monitor it instead of treating it. If surgery isn’t an option and you have symptoms, your provider may recommend treatments for MCD.
Multicentric Castleman disease (MCD) treatment
MCD is more difficult to treat than UCD. As it’s widespread, providers don’t typically use surgery or radiation to treat it. Instead, treatment depends on whether you have HHV-8 and how severe the disease is.
Your provider may use:
- Corticosteroids. These medications reduce inflammation and help provide symptom relief.
- Chemotherapy drugs. Anticancer medications slow the overgrowth of cells in your lymphatic system. Rituximab is a commonly prescribed medication used to treat HHV-8-associated MCD.
- Immunotherapy. This treatment includes monoclonal antibodies that help calm your body’s immune response. Siltuximab (Sylvant®) is the only iMCD therapy approved for use by the U.S. Food and Drug Administration (FDA).
- Antiviral drugs. You may need antiviral drugs to treat HIV or HHV-8 if you have HHV-8-associated MCD.
When should I see my healthcare provider?
Call a healthcare provider if you find a lump in your neck, armpit or groin.
Reach out to your provider if you experience other symptoms of Castleman disease that don’t go away after a few weeks.
Outlook / Prognosis
What is the life expectancy of someone with this disease?
The prognosis (outlook) is good for most people with UCD. Removing the affected lymph node is often enough to cure it. With treatment, UCD doesn’t usually affect life expectancy.
The outlook for people with MCD depends on the type of MCD and how serious it is. Some people have intense symptom flare-ups that can be life-threatening. Others have more chronic symptoms. Sixty-five percent to 75% of people diagnosed with MCD are still alive five years later. With breakthrough therapies, there’s hope that the outlook will continue to improve.
A note from Wockr
There aren’t easy answers when it comes to Castleman disease. Your experience will depend on the type of Castleman disease you have. Additional conditions like HIV or associated disorders — like TAFRO and POEMS — will also shape your experience. In some cases, surgery and careful monitoring may be the only treatment needed. Or you may need many treatments throughout your lifetime to prevent complications. Ask your healthcare provider how your unique diagnosis will impact your treatment and outlook.