Delirium
Delirium is a type of confusion that happens when illness, changes in your environment or other factors put too much stress on your brain. It’s more common in adults over 65. Delirium is a serious condition that can lead to long-term or even lasting problems, especially if not treated quickly. That’s why prevention is so important.
What Is Delirium?
Delirium is new or worsened confusion and changes to your mental abilities. It affects your thinking, memory, awareness and focus. It may cause you to act very differently than you typically would. It develops over hours to days.
It could go away if your doctor finds and treats the cause. But it may lead to ongoing issues with your thinking or memory. Delirium can be serious and lead to life-threatening complications in certain cases.
Types of delirium
There are three types:
- Hyperactive delirium: You feel disoriented, restless and agitated.
- Hypoactive delirium: You feel slowed, tired and confused.
- Mixed delirium: You switch between hyperactive and hypoactive symptoms.
Symptoms and Causes
Delirium symptoms
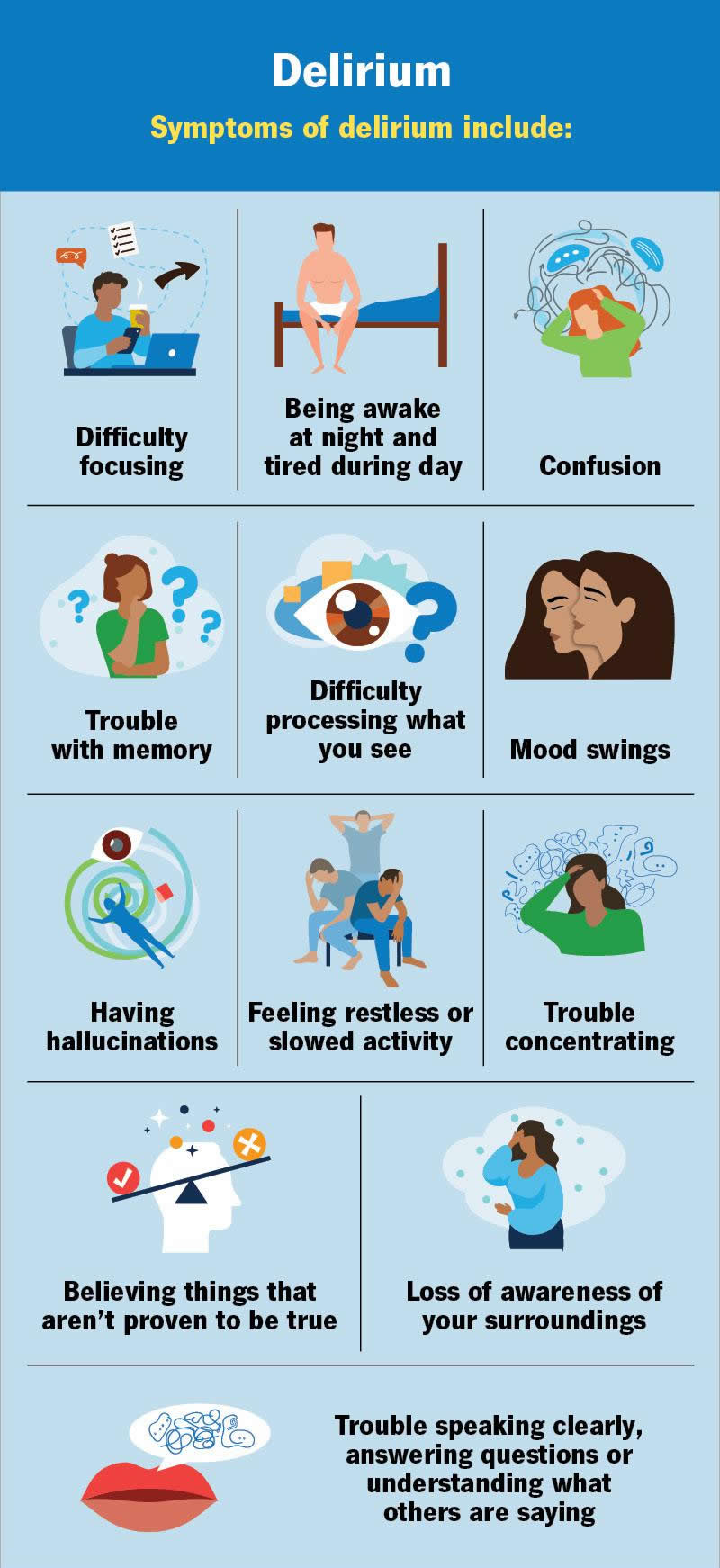
Symptoms of delirium include:
- Being awake at night and feeling tired during the day (sleep schedule change)
- Believing things that aren’t proven to be true (delusions)
- Confusion
- Difficulty focusing
- Difficulty processing what you see, including identifying objects
- Disorganized thinking and trouble concentrating
- Feeling restless (over excited) and/or slowed activity (difficulty staying alert)
- Loss of awareness of your surroundings (like the day, time, where you are, etc.)
- Mood swings (agitation, anger, depression, irritability)
- Problems remembering facts, events, people, etc.
- Seeing or hearing things that aren’t really there (hallucinations)
- Trouble speaking clearly, answering questions or understanding what others are saying
Symptoms can vary from person to person. They usually come and go, and they often feel worse at night than during the day.
Causes of delirium
Delirium happens when your body or brain is under too much stress. They have a hard time coping, which causes symptoms. This isn’t the same as everyday stress, like relationships, financial or work-related stress. Here are some examples of stressful triggers:
- A serious illness or infection
- Being in a room without windows or sunlight for a long time
- Certain medicines or taking too many medicines at once
- Medical equipment that keeps you in bed, like IVs or catheters
- New or sudden pain
- Not getting enough sleep
- Not moving around enough
- Surgery or a hospital stay
- Trouble seeing or hearing without glasses or hearing aids
- Using addictive substances
Delirium is possible during the end stages of life, especially for people receiving palliative care or hospice care.
Risk factors for delirium
You may be more at risk for delirium if you:
- Are above age 65 (but it can affect anyone at any age)
- Experience frailty
- Had delirium before
- Have a chronic health condition like heart or lung disease
- Have a mood disorder
- Have a substance use disorder
- Have memory issues like dementia
- Have trouble seeing or hearing
Complications of delirium
Complications may include:
- Aspiration pneumonia
- Bedsores (pressure ulcers)
- Weakness, leading to loss of mobility
- Falls and injuries like fractures
- Combative behavior
- Malnutrition and dehydration
- Cognitive impairment
- Loss of independence
- Dementia (new or worsening)
These may be short-term with treatment. Or they can be serious and even life-threatening, especially for people who are already sick. Each case is different.
Diagnosis and Tests
How doctors diagnose delirium
Your provider will make a diagnosis after:
- A physical exam
- A neurological exam
- Observing your behavior
- Learning more about your symptoms
- Reviewing your medical history
- Lab testing
What tests diagnose delirium?
There’s no test that shows if you have delirium. But tests play an important role in determining the cause of your delirium symptoms. Your provider might recommend the following tests:
- Blood tests
- Urinalysis
- Imaging tests (chest X-ray)
- Heart rhythm test (electrocardiogram)
- Lumbar puncture
- Brain scan (if needed)
These tests may also help your provider determine the best treatment for you.
Management and Treatment
How is delirium treated?
Treatment focuses on finding and managing the cause of your symptoms. Recovery takes time, but your provider may suggest ways to help you feel more comfortable (supportive therapy), like:
- Calm your mind: Listening to music, talking with loved ones or doing something creative may help reduce stress.
- Eat well and stay hydrated: Your body needs good nutrition and fluids to support recovery.
- Get enough sleep: Turn off the TV and keep the lights dim at night to help you sleep better.
- Limit changes: A familiar place may prevent confusion.
- Move safely: Light activity, like stretching or short walks (if you’re able), can help both your body and mind.
- Stay aware: Keep a calendar and clock nearby and rest near a window so you know where you are and what day it is.
- Use glasses and hearing aids: If you need them, wear them as recommended to stay connected to your surroundings.
Medications for delirium
There aren’t any FDA-approved medications available to treat delirium. But providers use medications to manage certain causes, like:
- Alcohol or substance withdrawal: Benzodiazepines may reduce symptoms.
- Infection: Antibiotics may treat a bacterial infection.
- Severe hyperactive delirium: Antipsychotics may prevent harm and reduce distress in certain cases.
- End of life: A variety of medications may ease pain.
Your provider will review how well you respond to these medications, usually on a daily basis. If there are side effects or you don’t need the medication anymore, your provider will stop it. Don’t make changes to your dose unless your provider tells you.
Outlook / Prognosis
What can I expect if I have delirium?
If you have delirium, changes in brain function can make it hard to understand what’s happening around you. It can also affect your memory, judgment and how you speak or act.
This condition is usually temporary, but symptoms can linger. This is more likely if you have a severe case. But even with quick treatment, some effects may last. Your provider can tell you more about what your situation looks like since it can vary from person to person.
Delirium life expectancy
Delirium doesn’t come with a set life expectancy like some other conditions do. But it’s a serious condition that can raise your risk of death, depending on factors like:
- Your age
- Underlying health conditions
- Where you’re receiving care (ICU, hospital, rehab, etc.)
- Any complications that arise
The outlook can vary widely, especially if delirium is severe or goes untreated. Your healthcare provider can give you the clearest picture based on your specific situation.
Prevention
Delirium prevention
Prevention for delirium may include:
- Watching for early signs: Providers will monitor those at a higher risk, especially in hospital settings.
- Using safer medications: Your care team will limit medications that may increase confusion.
- Maintaining good health: Keep your brain and body active, get enough sleep and socialize often.
- Educating loved ones: If you’re at high risk, teach your family and friends about the signs of delirium and how they can offer support.
A note from Wockr
Delirium can be frightening, both for you and for those by your side. Your loved one may say you seem like a completely different person. In some cases, especially near the end of life, it can be even more heartbreaking. But some cases of delirium aren’t permanent. If you get help quickly, your symptoms may get better. That’s why it’s so important to understand the signs, know the risk factors and take steps to prevent it whenever possible.