Diabetes-Related Retinopathy
While not everyone with diabetes will develop diabetes-related retinopathy, it’s still a major risk factor for vision loss. But diabetes and diabetes-related retinopathy are both manageable. Combining regular medical care and your own efforts can go a long way to maintaining your vision.
What Is Diabetes-Related Retinopathy?
Diabetes-related retinopathy is an eye disease that weakens the blood vessels in your retinas. The weakened blood vessels damage your retina. That can cause vision loss and even permanent blindness when the damage becomes severe enough.
Living with diabetes can be challenging. The possibility of developing diabetes-related retinopathy or learning you have it can make you feel even more worried. But you aren’t powerless. Not everyone with diabetes develops retinopathy. And there are several things you can do to help delay developing it. And even if you do develop it, there are ways to slow it and limit its severity.
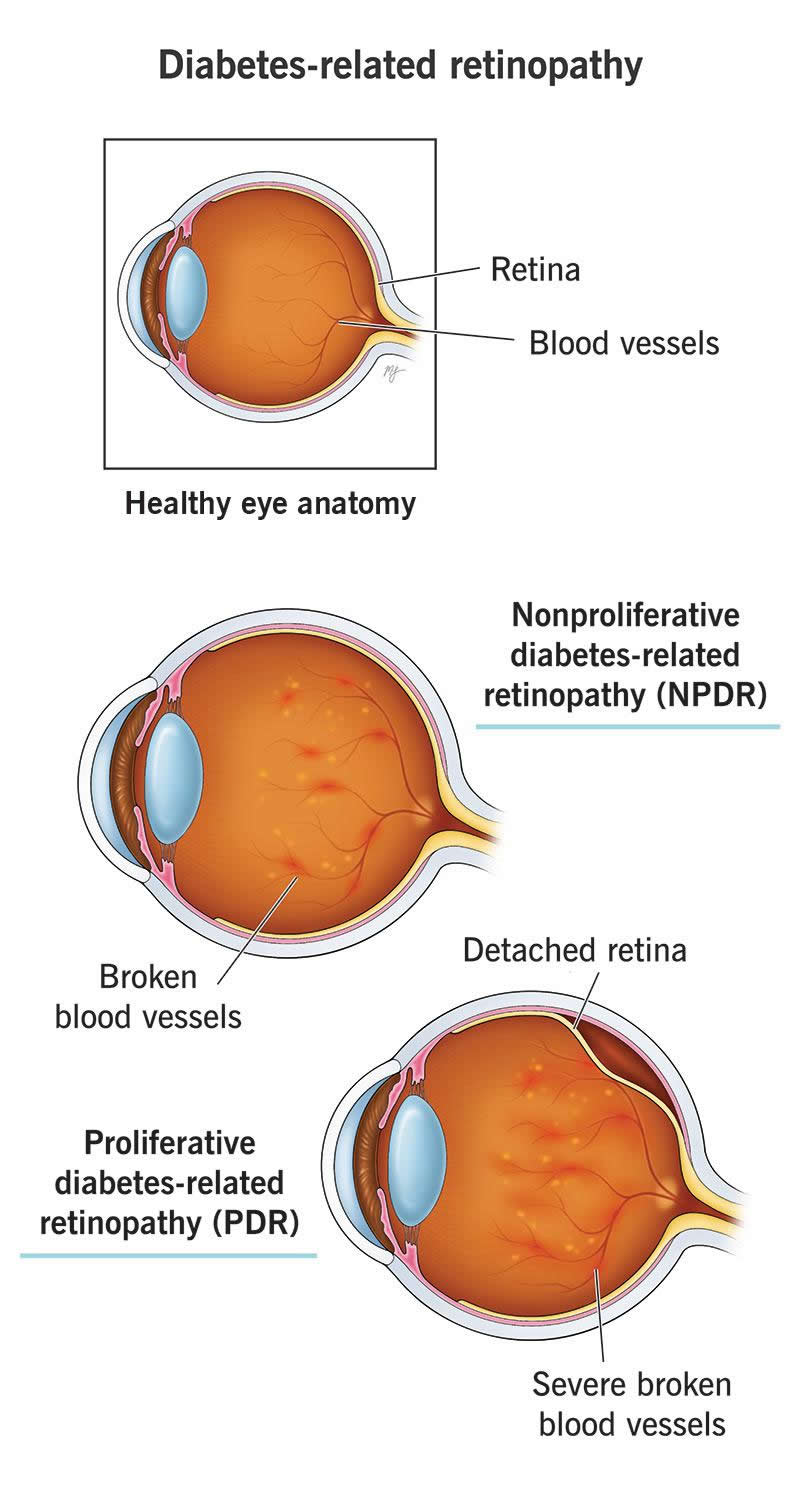
Stages of diabetes-related retinopathy
There are two stages of diabetes-related retinopathy:
- Nonproliferative diabetes-related retinopathy (NPDR). During this earlier stage of diabetes-related retinopathy, blood vessels leak into your retina. The damage to the blood vessels eventually makes them close off as your body tries to fix the damage.
- Proliferative diabetes-related retinopathy (PDR). Diabetes-related retinopathy gets worse over time. As it progresses, new blood vessels start to form to increase blood flow to undersupplied areas. But these vessels can leak blood and fluid into the vitreous, a gel-like liquid inside your eye. These blood vessels grow on the surface of your retina. Over time, the gel-like liquid can stick to these vessels and make them detach your retina, which can lead to blindness.
Symptoms and Causes
Symptoms of diabetes-related retinopathy
You might not have symptoms in the early stages of diabetes-related retinopathy. That’s because this condition doesn’t start causing vision changes until the damage is more severe or widespread throughout your retina.
Diabetes-related retinopathy symptoms can include:
- Blurred or distorted vision
- New color blindness or color vision changes (like colors looking faded or less vivid)
- Night blindness (nyctalopia)
- Eye floaters (myodesopsias) or streaks in your vision
- Blind spots (scotomas)
- Visual field defects
- Low vision and vision loss
Diabetes-related retinopathy causes
Diabetes-retinopathy can happen because of multiple types of diabetes. They include:
Diabetes causes increased blood sugar levels and can damage the insides of blood vessels throughout your body over time. When you have diabetes-related retinopathy, damaged blood vessels in your retina are trying to repair and reroute to avoid an interruption in blood supply. As a result, fragile new blood vessels grow on the surface of your retina. These new blood vessels can cause retinal detachments and bleeding into the vitreous, a gel-like fluid in your eye. The damaged blood vessels can also leak fluid into your retina, causing macular edema. This can cause blurry vision.
Risk factors
Risk factors for diabetes-related retinopathy include:
- Difficult-to-manage diabetes
- High blood pressure (hypertension)
- High cholesterol (hyperlipidemia)
- Heart-specific cardiovascular diseases, like heart disease and coronary artery disease
- Chronic kidney disease and kidney failure
Complications of diabetes-related retinopathy
Complications of diabetes-related retinopathy include:
- Diabetes-related macular edema
- Retinal detachments
- Vitreous hemorrhage
- Glaucoma
- Macular ischemia (loss of blood flow to the part of the retina responsible for color and sharp vision)
Eventually, complications of diabetes-related retinopathy can cause so much damage that the light-detecting cells, known as photoreceptors, stop working correctly. When that happens to enough photoreceptors, it causes permanent vision loss and can eventually lead to blindness.
Diagnosis and Tests
How is it diagnosed?
Many of the key changes that happen with diabetes-related retinopathy don’t cause symptoms until much later. But they’re still visible very early on to an eye care specialist who looks at the back of your eyes using special instruments during a dilated eye exam.
Those changes can include:
- Cotton wool spots
- Retinal hemorrhages (bleeding)
- Microaneurysms (small blood vessels that bulge and burst)
- Neovascularization of the eye
- Macular edema
- Retinal exudates (lipid deposits)
- Abnormal-looking retinal blood vessels
- Vitreous hemorrhage (bleeding into the gel-like fluid)
Management and Treatment
How is diabetes-related retinopathy treated?
Diabetes-related retinopathy is treatable but not curable. Some of the symptoms or retinal changes are treatable. But certain types of damage aren’t reversible once they become severe enough.
The two main approaches are managing your diabetes and eye treatments. Your provider will recommend treatments for both of them.
Managing your diabetes
Research clearly ties higher blood sugar and hemoglobin A1C levels to diabetes-related retinopathy. So, managing your blood sugar — keeping it lower and more consistent — is critical to delaying and slowing how diabetes-related retinopathy progresses and affects your retinas.
Key parts of managing your diabetes include:
- Monitoring your blood sugar. You can do this with blood glucose testing methods, like finger-stick testing or devices that can provide continuous glucose monitoring.
- Managing what you eat. The foods you eat directly affect your blood sugar and A1C.
- Taking prescribed medications. If your healthcare provider prescribes medications for your diabetes, take them as directed. It can make a huge difference in keeping your blood sugar and A1C within — or at least close to — your recommended range.
- Getting regular physical exams (check-ups). These are essential for monitoring your general health. They can also catch important health and body changes before you ever feel any symptoms.
- Keeping up with regular eye exams as recommended. If you have diabetes or prediabetes, regular eye exams are critical. They can help you get treatment before any changes become permanent.
- Reach and maintain a weight that’s healthy for you. This can be a big help in managing your diabetes. Your primary care provider can guide you as you do this.
Eye treatments
Eye treatments focus on managing vision and eye symptoms and limiting or slowing retinal damage. Some specific treatments for diabetes-related retinopathy include:
- Medications. Examples include anti-vascular endothelial growth factor (anti-VEGF) drugs or corticosteroids. Your eye doctor can explain other available medication options.
- Laser surgery. During procedures like laser photocoagulation, your eye specialist uses a laser to treat your retina to prevent blood vessel growth, shrink abnormal vessels or stop leaking. But sometimes, this leads to loss of night vision or peripheral vision.
- Eye surgeries. Your healthcare provider may recommend a vitrectomy if your retina is detached, if you have vitreous hemorrhage that won’t clear or have certain other types of retina damage.
When should I see my healthcare provider?
If you have diabetes or diabetes-related retinopathy, it’s crucial that you see an eye care specialist regularly. They’ll recommend a schedule for regular follow-up visits, which can make a big difference when it comes to catching more serious changes before they’re severe or permanent.
You should also call or see your provider if you notice any gradual vision changes like:
- Vision loss or trouble seeing as well as you used to
- Blurred or distorted vision
- Areas in your vision that look dim, faded or different from how you saw before
You should go to the nearest hospital or emergency room if you have SUDDEN vision changes like:
- Severe eye pain
- Complete loss of vision or severe loss of vision
Outlook / Prognosis
What can I expect if I have diabetes-related retinopathy?
Diabetes-related retinopathy is a permanent, lifelong condition. There isn’t a cure, but you can take steps to manage it and limit loss of vision.
Diabetes-related retinopathy is likely to happen to people with diabetes, but having diabetes doesn’t guarantee you’ll develop it. Still, it’s important to do everything you can to avoid or delay it because it can so heavily impact your life.
With early diagnosis and timely treatment, you may be able to prevent vision loss and delay diabetes-related retinopathy progression. After diabetes-related retinopathy treatment, you’ll have the best chance of limiting or delaying the effects of this disease if you manage your diabetes and keep your blood sugar within ranges that your providers recommend.
Unfortunately, some people will still develop more severe complications. But there are ways to delay those complications as long as possible and manage diabetes-related vision changes. Anything you can do to limit the severity of any vision changes is preferable to developing more severe issues or changes early on.
Prevention
Can diabetes-related retinopathy be prevented?
Yes, managing your blood sugar levels and maintaining a low hemoglobin A1C can help you prevent diabetes-related retinopathy. Doing these can also make retinopathy regress over time.
Not everyone with diabetes has it, but the odds of developing diabetes-related retinopathy are significantly higher in people with unmanaged blood sugar levels and in people who have diabetes over a longer period of time.
If you don’t have diabetes but have a high chance of developing it (such as having prediabetes), you can act long before you might receive a diabetes diagnosis. Acting earlier can prevent and delay when or if you develop diabetes, which can affect when or if you develop diabetes-related retinopathy.
Eye exams can catch early signs of diabetes-related retinopathy long before you have symptoms. If you have other family members, especially first-degree biological relatives (parents, siblings or children) with diabetes, you have a much higher risk of having it, so regular eye exams are especially important for you.
A note from Wockr
No matter how well you manage your diabetes, sometimes, it isn’t enough to prevent diabetes-related retinopathy from happening. Managing your diabetes and regular vision exams and eye care are still key, though. They can help you maintain and preserve your vision.
Your diabetes-related healthcare provider can guide you on this and refer you to an eye specialist. With regular care and support, there’s a lot you can do to safeguard your vision.