Dilated Cardiomyopathy
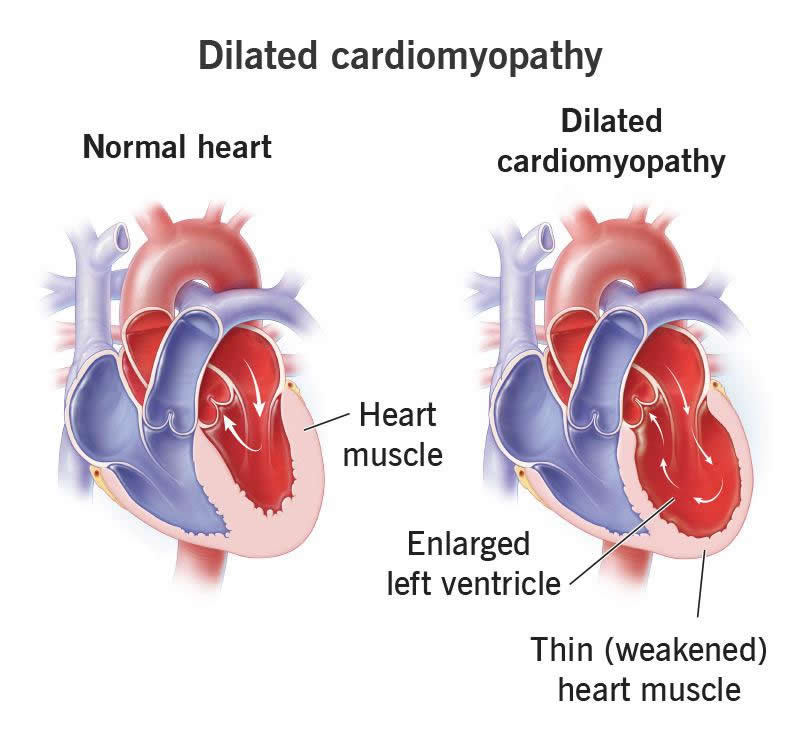
Dilated cardiomyopathy causes tissue in your heart’s main pumping chamber to expand (dilate) and thin out. This makes it unable to pump as strongly as it should. Genetics or heart attack damage can cause this, but often, the cause is unknown. This condition can affect several chambers of your heart and lead to complications like heart failure.
Overview
What is dilated cardiomyopathy?
Dilated cardiomyopathy is an issue with your heart muscle stretching out and becoming larger than usual. It starts in your heart’s main pumping chamber (left ventricle). In severe cases, it affects more areas of your heart.
With increased wall stress, the tissue in your left ventricle becomes enlarged and then thins. This causes it to pump with less force than it should. After each beat, more blood remains in your heart. This makes it increasingly difficult to keep up with your body’s needs.
Researchers estimate that 36 people per 100,000 in the general population have dilated cardiomyopathy.
Fortunately, treatments are available for this heart condition. And there are things you can do to help manage this condition.
Symptoms and Causes
What are the symptoms?
Many people with dilated cardiomyopathy don’t have any symptoms, especially in the early stages. But as heart function worsens, you may notice symptoms more and more.
Dilated cardiomyopathy symptoms may include:
- Chest pain
- Cough and congestion
- Dizziness or lightheadedness
- Fainting
- Fatigue (unusual tiredness)
- Palpitations or fluttering in your chest
- Shortness of breath (dyspnea)
- Swelling in your belly, legs, ankles and feet (edema)
- Unexpected weight gain from fluid retention
What causes dilated cardiomyopathy?
In many cases, experts don’t know the cause. In others, dilated cardiomyopathy causes may include:
- Abnormal heart rhythms (arrhythmia)
- Alcohol use disorder
- Certain chemotherapy drugs that are toxic to your heart (cardiotoxic)
- Complications in the late stages of pregnancy or shortly after childbirth
- Congenital heart disease
- Coronary artery disease
- Diabetes
- Genes you get from a biological parent (familial dilated cardiomyopathy), which may account for more than 50% of cases
- Heart attack
- Heart valve disease
- High blood pressure
- HIV
- Infection like myocarditis
- Recreational drugs like cocaine
- Thyroid disease
- Viral hepatitis
Some people have more than one cause. For example, you can be at risk because of genetics and then get a medical condition that leads to dilated cardiomyopathy.
What are the risk factors?
You may be more at risk for dilated cardiomyopathy if you:
- Are younger than 50
- Are Black
- Are male
- Have dilated cardiomyopathy in your biological family
What are the complications of dilated cardiomyopathy?
In advanced stages, dilated cardiomyopathy can lead to complications.
These complications may include:
- Abnormal heart rhythms (arrhythmia)
- Angina (chest pain)
- Blood clots in your heart, which can also travel to a lung and become a pulmonary embolism
- Cardiac arrest
- Heart attack
- Heart failure
- Heart valve disease
- Stroke
Diagnosis and Tests
How is dilated cardiomyopathy diagnosed?
A healthcare provider will start by taking your medical history and family history. They’ll perform a physical exam that may include listening to your lungs to check for fluid build-up. Your provider may hear a heart murmur before you even have symptoms.
Testing will determine the severity and help healthcare providers plan your dilated cardiomyopathy treatment.
What tests will be done to diagnose dilated cardiomyopathy?
Tests you may need include:
- Angiogram to look for narrow areas in your coronary arteries, which send blood to your heart
- Blood tests like one that checks for heart damage
- Chest X-ray to see if your heart looks larger than a typical heart
- Echocardiogram to show how well your heart works
- Electrocardiogram (EKG) to check for abnormal heart rhythms
- Exercise stress test to see the impact of physical activity on your heart
- Genetic testing to find out if you inherited cardiomyopathy
- Heart MRI to show your ventricles’ size and function
- Endomyocardial biopsy (rarely used to examine a tissue sample)
Management and Treatment
How is dilated cardiomyopathy treated?
You may need a variety of dilated cardiomyopathy treatments. In most cases, they won’t cure the disease, but they can help you manage the symptoms and live longer. Treating dilated cardiomyopathy may involve medicines, changes to your lifestyle or surgeries. The earlier you start treatment, the better your prognosis (outcome). Your cardiologist or heart failure specialist will work with you to find the right combination of these medicines.
Medicines
Medications that improve your heart function with dilated cardiomyopathy include:
- ACE inhibitors
- Aldosterone antagonists
- Angiotensin receptor/neprilysin inhibitors (ARNI)
- Antiarrhythmics to treat abnormal heart rhythms
- Beta-blockers
- Blood thinners (anticoagulants) for people with atrial fibrillation
- Diuretics
Changes in daily habits
Changes to your daily routine can improve how well medications work and possibly help you delay or avoid the need for a procedure.
These changes include:
- Protecting your body: You can improve your health by limiting how many alcohol-containing drinks you have, avoiding recreational drugs and protecting yourself from viral hepatitis and HIV.
- Eating heart-healthy foods: Lean proteins, like chicken and fish, and plenty of fruits and vegetables are good for your heart. Low-salt foods can prevent fluid build-up that strains your heart.
- Increasing physical activity: Gentle exercises can improve heart function. A cardiac rehabilitation program provides a safe environment for getting started.
Surgery and minimally invasive procedures
You may need a procedure or surgery if you have advanced dilated cardiomyopathy and limited heart function. Procedures for dilated cardiomyopathy treatment include:
- Biventricular pacemaker to help your heart pump more regularly
- Implantable cardioverter defibrillator (ICD) to send a shock that returns your heart rhythm to normal when you need it
- Heart failure surgery or heart valve surgery to improve your heart function
- Left ventricular assist device (LVAD) to help your weakened heart muscle pump blood
- Heart transplant (a rare option for when other treatments don’t work)
Outlook / Prognosis
What can I expect if I have dilated cardiomyopathy?
Your prognosis depends on the cause and severity of the disease. With ongoing care, you may return to work and your usual daily activities. But you may have symptoms that get worse with time. Advanced dilated cardiomyopathy or complications can make you severely ill. You may need to stay in the hospital until symptoms improve.
Dilated cardiomyopathy can get worse for many people and lead to long-term heart failure. This means your heart can’t keep up with the demands on it. Kidney failure and severe heart failure are signs of a poor prognosis (outcome). People who have symptoms at rest or can’t do physical activity tend to have the worst prognosis.
Still, the prognosis for people with dilated cardiomyopathy has improved in recent years. This is due to the treatments available and early diagnosis and treatment. Today, more than 80% of people with this condition are alive at their eight-year follow-up visit and don’t need a heart transplant.
Prevention
Can this be prevented?
It’s not always possible to prevent this condition. It may run in your biological family or be a side effect of a treatment like chemotherapy.
But you may be able to prevent dilated cardiomyopathy by:
- Avoiding cocaine
- Consuming alcohol-containing beverages in moderation
- Managing conditions like diabetes and high blood pressure
- Taking good care of your heart to prevent a heart attack
Living With
How do I take care of myself?
You can care for yourself by following your provider’s instructions. These include:
- Checking daily for signs of potential complications like sudden weight gain
- Committing to changes your provider suggests, like eating low-salt foods
- Seeing your healthcare provider a few times a year for follow-up visits
- Taking medications as prescribed
When should I see my healthcare provider?
Because your condition can change over time, your best game plan is to have regular visits with your provider. These visits should continue for the rest of your life. Contact your provider if the symptoms get worse. They can offer treatments that help you manage symptoms.
What questions should I ask my healthcare provider?
You may have lots of questions about a condition that’s new to you, like:
- Does my family need to get genetic testing?
- Do I need to avoid strenuous activity?
- Is there a support group I can join locally or online?
A note from Wockr
No one wants to learn that their heart isn’t working as well as it should. But today, healthcare providers can offer various treatments to help your heart work better if you have dilated cardiomyopathy. And there are simple changes you can make to improve your situation, too. Don’t be afraid to ask questions so you can understand your options. You can work with your provider to find a way forward.