Graves’ Disease
Graves’ disease is an autoimmune disease that affects your thyroid gland. The gland produces too much thyroid hormone, a condition known as hyperthyroidism. An overactive thyroid causes problems with your heart and bones. Treatments can help.
What Is Graves’ Disease?
Graves’ disease is a lifelong (chronic) autoimmune disease that causes your thyroid to make too much thyroid hormone. It happens because your body makes antibodies to your thyroid gland.
It’s one of the most common causes of hyperthyroidism (overactive thyroid), especially if you have a family history of thyroid problems. Graves’ disease mainly affects your thyroid. But it can also affect your eyes and skin.
Graves’ disease speeds up your metabolism. This can affect several aspects of your health. You may not feel like yourself or even feel out of control of your body. It’s important to get medical treatment if you develop signs of this condition.
Symptoms and Causes
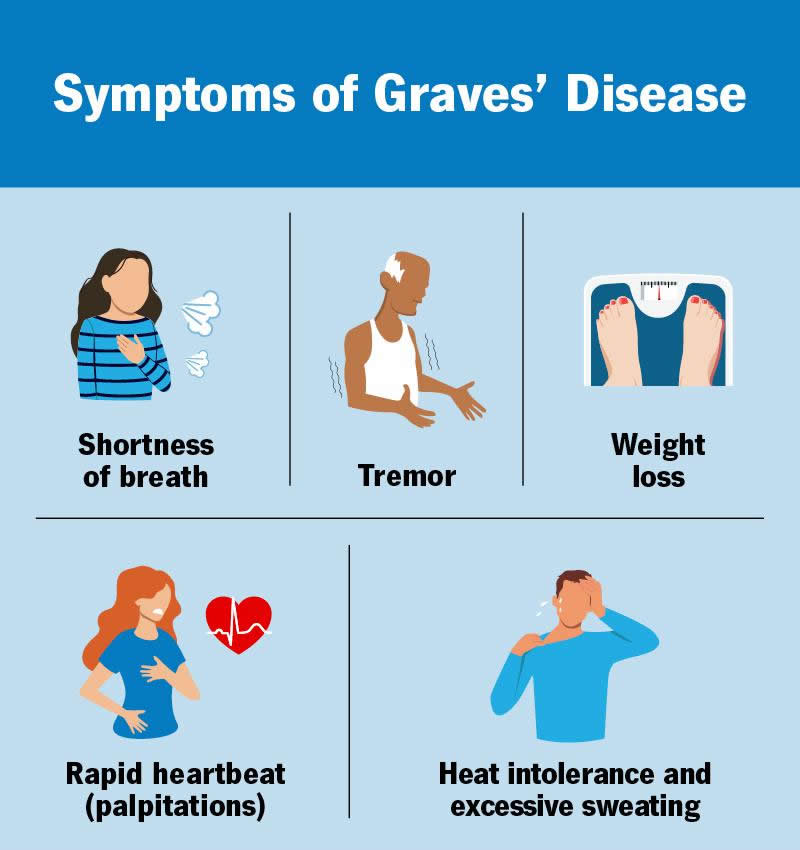
Symptoms of Graves’ disease
Symptoms of Graves’ disease (and hyperthyroidism) include:
- Heat intolerance and excessive sweating
- Rapid heartbeat (tachycardia)
- Shortness of breath (dyspnea)
- Tremor (shakiness)
- Anxiety or nervousness
- Diarrhea and/or pooping more frequently
- Enlarged thyroid gland (goiter)
- Hair loss
- Insomnia
- Light menstrual bleeding or fewer or absent periods
- Thin, warm and moist skin
- Weight loss
The onset of Graves’ disease symptoms is usually gradual. It often takes several weeks or months to develop. But sometimes, it develops suddenly over a few days. You may experience some of these symptoms or many at the same time.
See your healthcare provider if you have symptoms. Graves’ disease needs to be treated.
Other symptoms related to Graves’ disease
Graves’ disease can also cause eye issues, like:
- Bulging eyes
- Double vision
- Gritty, irritated eyes
- Light sensitivity (photophobia)
- Pressure or pain in your eyes
This is called Graves’ orbitopathy or thyroid eye disease. About 1 in 3 people with Graves’ disease develop it.
Up to 4% of people with Graves’ disease develop pretibial myxedema (Graves’ dermopathy). It causes a lumpy, discolored thickening of your skin — usually on your legs.
About 1% of people with Graves’ disease have thyroid acropachy. This causes clubbing of your fingers and toes.
Graves’ disease cause
Graves’ disease happens when something triggers your immune system to overproduce an antibody called thyroid-stimulating immunoglobulin (TSI). TSI attaches to healthy thyroid cells, causing your thyroid to overproduce thyroid hormones.
In one study, researchers estimated that your genes contribute to 79% of your risk of developing Graves’ disease. This means that Graves’ disease is partially hereditary. The remaining percentage of risk (21%) is due to environmental factors.
Scientists don’t know exactly why your immune system attacks your thyroid. But they think the trigger may happen due to environmental factors, like:
- Stress
- Pregnancy and the postpartum period
- Viruses and infections
Risk factors
Risk factors for Graves’ disease include:
- A biological family history of Graves’ disease
- Having another autoimmune condition, like Type 1 diabetes or pernicious anemia
- Having estrogen as your main sex hormone
- Selenium and vitamin D deficiencies
- Smoking
Complications of Graves’ disease
Untreated or undermanaged Graves’ disease increases your risk of the following complications:
- Heart problems. Graves’ disease can cause atrial fibrillation (Afib). This increases your risk of heart failure and stroke.
- Osteoporosis. This condition makes your bones thinner and less dense. It can lead to repeated bone fractures.
- Thyroid storm. This happens when your thyroid releases a bunch of thyroid hormone in a short amount of time. It’s a rare complication that’s life-threatening.
Graves’ disease may also increase your risk of thyroid cancer.
Untreated Graves’ disease during pregnancy can be harmful to you and the fetus. It can increase the risk of:
- Congestive heart failure in the mother
- Miscarriage
- Preeclampsia
- Premature labor
- Low birth weight
- Infant hyperthyroidism
Diagnosis and Tests
How doctors diagnose Graves’ disease
Your healthcare provider will ask about your symptoms and medical history. This includes your family history of thyroid disease. They’ll also do a physical exam.
They may also recommend the following tests to confirm a Graves’ disease diagnosis:
- Thyroid blood tests. These tests check the level of thyroid hormone and thyroid-stimulating hormone (TSH) in your blood.
- Thyroid antibody blood tests. These tests check for the antibodies linked with Graves’ disease.
- Thyroid uptake and scan. In this test, you swallow a small amount of radioactive iodine. If your thyroid absorbs a lot of the iodine, it can be a sign of Graves’ disease.
- Doppler ultrasound. This test checks for increased blood flow in your thyroid due to Graves’ disease. You may need this test if radioactive iodine uptake isn’t safe due to pregnancy or breastfeeding.
Management and Treatment
How is Graves’ disease treated?
Graves’ disease is a lifelong (chronic) condition. But treatments can keep your thyroid hormone levels in check. Medical care may even make the disease temporarily go away (remission).
Treatments for Graves’ disease include:
- Beta-blockers: Beta-blockers, like propranolol and atenolol, are often the first line of treatment for Graves’ disease. These medications regulate your heart rate until other hyperthyroidism treatments take effect.
- Antithyroid medications: Antithyroid medications, like methimazole and propylthiouracil, block thyroid hormone production.
- Radioiodine therapy: This therapy slowly destroys thyroid gland cells. As your thyroid gland shrinks, hormone levels return to normal. But you’ll likely eventually develop hypothyroidism.
- Surgery: A thyroidectomy involves surgically removing all or part of your thyroid gland.
Radioiodine therapy and thyroidectomy usually lead to hypothyroidism (underactive thyroid). If you develop this condition, you’ll need to take thyroid replacement hormone medications for the rest of your life. But hypothyroidism is easier to treat than hyperthyroidism. It causes fewer long-term health problems.
All the Graves’ disease treatment options have benefits and risks. And there’s no agreement in the medical community on which treatment is the best. It’s important to discuss all the options in detail with your provider to make the best choice for you.
Researchers are currently studying antigen-specific immunotherapy as a treatment for Graves’ disease. Ask your healthcare provider if a clinical trial is an option.
When should I see my healthcare provider?
You’ll need to see your healthcare provider regularly throughout your life. They’ll make sure your thyroid levels are in check and your treatment plan is working. If you develop any new symptoms, talk to your provider.
If you’re experiencing symptoms of thyroid storm, call 911 (or your local emergency service number) or get to the nearest emergency room (ER) as soon as possible. Thyroid storm is life-threatening.
Outlook / Prognosis
What can I expect if I have this condition?
If Graves’ disease is properly treated, the prognosis (outlook) is generally good. Without treatment, Graves’ disease can cause complications that can affect your overall health or life expectancy.
A note from Wockr
Getting a new diagnosis can be stressful. The good news is that Graves’ disease is a manageable and treatable condition. If you have symptoms or certain risk factors, like a family history of thyroid disease, contact your healthcare provider. They can recommend some simple tests to see if your thyroid is making too much thyroid hormone.