Indigestion (Dyspepsia)
Occasional indigestion (dyspepsia) is common and not serious. If you get a stomachache after a large meal, you can usually relieve it with an antacid. But if you have indigestion often, there might be more going on. Sometimes, it means you have a treatable condition, like acid reflux or peptic ulcer disease. Other times, it’s more complex.
What Is Indigestion (Dyspepsia)?
Indigestion is pain or discomfort that happens while your stomach digests food. It’s also called dyspepsia, which means impaired digestion. If you often get a stomachache after eating, something in your digestion may not be working as it should.
Indigestion isn’t usually serious — small changes in your eating habits can help. But how often it happens and how severe it feels matter.
Most people have occasional indigestion. For others, it happens often enough to affect daily life. If that’s the case, you may want to see a healthcare provider. Sometimes, indigestion is a sign of an underlying digestive condition. Other times, there’s no clear cause.
Symptoms and Causes
What are indigestion symptoms?
Healthcare providers define indigestion (dyspepsia) by the following three symptoms:
- Pain in your upper belly: This area, called the epigastric region, holds important digestive organs like your stomach, liver, pancreas and the first part of your small intestine.
- A burning feeling: This can come from stomach acid, digestive enzymes or inflammation. You might feel it in your upper belly or chest.
- Uncomfortable fullness: You may feel full sooner than expected, or long after eating. This can make it hard to eat even small amounts.
Symptoms often show up within minutes to a few hours after a meal. It normally takes three to five hours for your stomach to digest food before passing it to your small intestine. During this time, your pancreas and gallbladder release enzymes and bile to help break food down — right in the same area where indigestion pain tends to show up.
Many people who experience indigestion also report additional symptoms, including:
These symptoms can overlap with dyspepsia, or they may occur on their own.
Sometimes, a heart attack can feel like indigestion — called a silent heart attack.
Seek emergency care if you have indigestion along with:
- A tight, clenching feeling in your diaphragm
- Pain in your jaw, arms or upper back
- Fatigue
- Shortness of breath
- Chest heaviness or soreness
- Sweating
What causes indigestion (dyspepsia)?
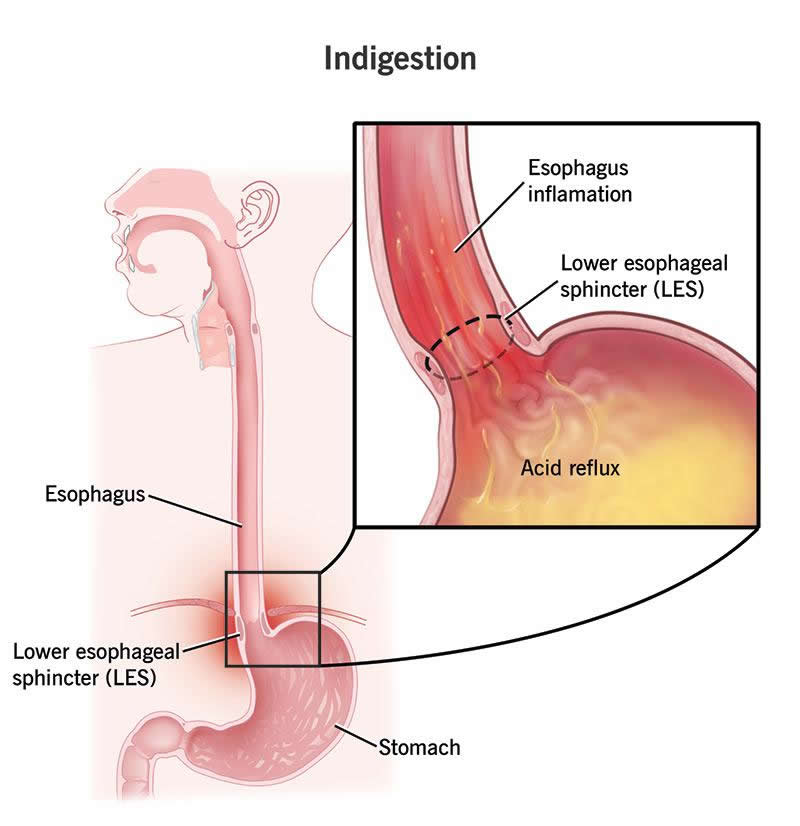
The most common cause of indigestion is stomach acid — especially when there’s too much of it or when it gets where it doesn’t belong. Acid can irritate the lining of your stomach, esophagus or small intestine, causing that familiar burning or painful sensation.
This extra acid often results from underlying conditions like GERD (acid reflux) or peptic ulcer disease, which are among the most common causes of chronic indigestion.
But indigestion can also stem from what and how you eat, how well your digestive system functions and how your nerves interpret discomfort in your gut.
Occasional indigestion
Sometimes, indigestion is simply due to overeating or eating rich, fatty foods. These meals require more digestive effort, which means more acid and stronger contractions from your stomach, gallbladder and pancreas. This extra activity can irritate your digestive tract and cause temporary discomfort.
Chronic indigestion
When indigestion happens regularly, it may be linked to a digestive condition — or it may have no identifiable cause.
- GERD allows acid to escape from your stomach into your esophagus, which isn’t built to handle it.
- Peptic ulcers can form in your stomach or the first part of your small intestine (duodenum) when acid damages the protective lining.
- Gastritis occurs when acid irritates or inflames the stomach lining.
These acid-related conditions are among the few clear “organic” causes of indigestion. When symptoms like heartburn, regurgitation or belching appear alongside dyspepsia, GERD is often the reason. If nausea, early fullness or bloating are present, peptic ulcer disease may be the cause.
When testing rules out acid-related disease, the diagnosis is often functional dyspepsia — a condition where overly sensitive gut nerves misinterpret normal digestion as pain or discomfort.
Risk factors
You’re more likely to experience indigestion if you have certain conditions or lifestyle factors that affect your digestive system or increase acid production:
Health conditions linked to dyspepsia include:
- Eating disorders
- Food intolerances
- Gallstones
- Gastroparesis
- Hiatal hernia
- H. pylori infection
- IBS
- SIBO
- Stomach cancer
- Visceral hypersensitivity
Lifestyle factors that may raise your risk include:
- Chronic stress
- Smoking
- Frequent alcohol use
- Regular use of NSAIDs (like ibuprofen)
- An eating pattern high in fried, spicy or acidic foods
Specific food triggers include:
- Carbonated drinks
- Coffee
- Chocolate
- Greasy or fried foods (like fried chicken)
- Shellfish (like shrimp and lobster)
- Spicy foods
Diagnosis and Tests
How is dyspepsia diagnosed?
If your indigestion is mild or only happens once in a while, you probably don’t need a formal diagnosis. But if it’s frequent, severe or interfering with your daily life, your provider will start by asking about your symptoms.
They’ll likely begin with:
- A physical exam
- A review of your health history
- Questions about your eating habits and lifestyle
In some cases, your provider may prescribe acid-blocking medication first to see if it helps. If it does, your symptoms are likely related to stomach acid. If it doesn’t — or if you have other concerning symptoms — your provider may recommend further testing to check for an underlying condition.
Tests might include:
- Imaging tests
- Blood tests
- Breath tests (to check for H. pylori)
- Stool tests
- Upper endoscopy (to view your esophagus, stomach and small intestine)
If tests don’t show any clear cause and acid-reducing medications don’t help, your provider may diagnose functional dyspepsia.
Management and Treatment
How can I treat indigestion at home?
If your symptoms are mild or occasional, you can often manage them with simple changes:
- Adjust your eating habits: Eat smaller meals and avoid rich or fatty foods, which require more stomach acid to digest. Try to finish eating a few hours before bedtime.
- Review your medications: If you regularly take NSAIDs (like ibuprofen), they may irritate your stomach. Talk to your provider about other options for pain relief.
- Sip water: Small sips may help wash acid out of your esophagus or help your stomach empty more quickly. But too much water can sometimes make symptoms worse.
- Use antacids: Over-the-counter antacids can neutralize stomach acid and relieve occasional indigestion. But if you need them often — or they don’t work — see your provider.
How do healthcare providers treat chronic indigestion?
If you have traditional acid-related indigestion, your provider may prescribe medications to reduce or manage stomach acid. These can include:
- Antibiotics: Used to treat bacterial infections like H. pylori or SIBO, which can contribute to indigestion.
- H2 blockers: These reduce stomach acid by blocking histamine signals. They’re effective in the short term but may lose effectiveness with long-term use.
- Prokinetic agents: These help your digestive system move food along more quickly, reducing how long acid and enzymes sit in your stomach.
- Proton pump inhibitors (PPIs): These are strong acid blockers that also help heal tissue damage, such as ulcers or inflammation.
If you have functional dyspepsia, treatment may involve a combination of:
- Medications
- Eating habit changes
- Lifestyle changes
- Complementary therapies (like stress management or probiotics)
It may take some trial and error to find what works best for you.
When should I seek healthcare for indigestion?
See a healthcare provider if your symptoms are frequent, if antacids don’t help or if you’re relying on antacids too often and need a longer-term plan. You should also seek care if your current treatment stops working or if you develop new or concerning symptoms.
Red-flag symptoms include:
Outlook / Prognosis
Is dyspepsia curable?
Not all causes of indigestion are curable, but most are treatable. Depending on the underlying issue, you may need occasional or daily treatment — sometimes long-term.
Medications that reduce stomach acid are often effective, but they can have side effects. You may need to work with your provider to find the right balance.
Functional dyspepsia can be harder to treat, and not everyone finds lasting relief.
A note from Wockr
Indigestion is common and usually not serious. But when it happens often, it can interfere with your eating, sleeping and overall quality of life. It may be a sign of an underlying condition — and in rare cases, a serious one.
Your digestive system is complex. An experienced healthcare provider can help you figure out what’s going on and guide you toward relief.