Insulin Resistance
Insulin resistance is a complex condition in which your body doesn’t respond as it should to insulin. Insulin is a hormone your pancreas makes that’s essential for regulating blood sugar levels. Several genetic and lifestyle factors can contribute to insulin resistance.
Overview
What is insulin resistance?
Insulin resistance happens when cells in your muscles, fat and liver don’t respond to insulin as they should. This is also known as impaired insulin sensitivity. Insulin is essential for life and regulating blood glucose (sugar) levels.
Insulin helps move glucose from your blood into your cells so your body can use it for energy. For several reasons, your cells can respond inappropriately to insulin. This means they can’t efficiently use the glucose for energy or for storage. As a result, glucose continues to build up in your blood. Your pancreas makes more insulin to try to overcome your increasing blood glucose levels. This is called hyperinsulinemia.
As long as your pancreas can make enough insulin to balance out your blood sugar levels, they’ll stay in a healthy range. If your cells become too resistant to insulin, it leads to elevated blood glucose levels (hyperglycemia).
Over time, hyperglycemia can lead to prediabetes and Type 2 diabetes.
The condition is also associated with:
- Obesity
- Cardiovascular disease
- Metabolic dysfunction-associated steatotic liver disease
- Metabolic syndrome
- Polycystic ovary syndrome (PCOS)
Who does insulin resistance affect?
Insulin resistance can affect anyone — you don’t have to have diabetes — and it can be temporary (for example, using steroid medication for a brief period causes insulin resistance) or chronic. The two main factors that seem to contribute to insulin resistance are excess body fat, especially around your belly, and a lack of physical activity.
Having a family history of insulin resistance (family members with prediabetes, type 2 diabetes, and/or PCOS) can also contribute to insulin resistance.
People who have prediabetes and Type 2 diabetes usually have insulin resistance. People with Type 1 diabetes can also experience insulin resistance.
Symptoms and Causes
What are the symptoms of insulin resistance?
If you have insulin resistance, but your pancreas can increase insulin production to keep your blood sugar levels in range, you won’t have any symptoms.
But over time, the condition can get worse, and the cells in your pancreas that make insulin can wear out. Eventually, your pancreas can’t produce enough insulin to overcome it, leading to elevated blood sugar.
People with consistently high blood sugar levels can experience the following symptoms:
- Unexplained weight loss
- Fatigue
- Increased thirst
- Frequent urination (peeing)
- Increased hunger
- Blurred vision
- Yeast infections
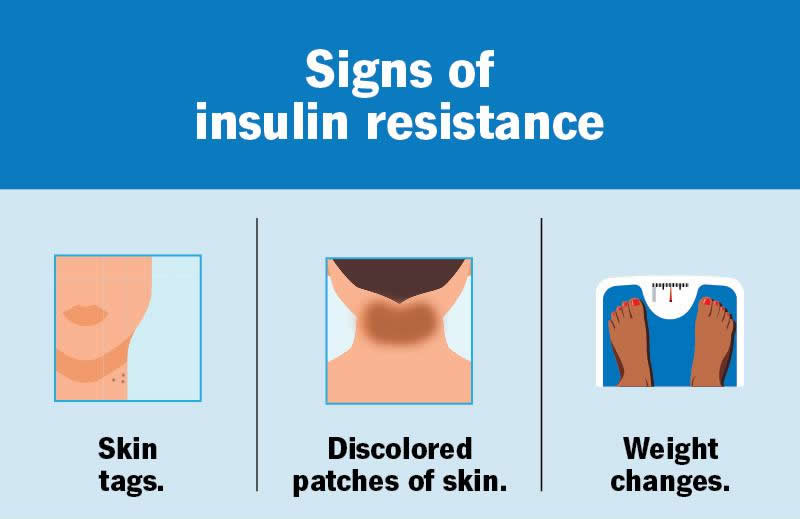
Many people have no symptoms of prediabetes, often for years. Prediabetes may be invisible until it develops into Type 2 diabetes. Some people with prediabetes may experience the following symptoms:
- Darkened skin in your armpit or back and sides of your neck, called acanthosis nigricans
- Skin tags
- Eye changes that can lead to diabetes-related retinopathy
If you’re experiencing any of these symptoms, it’s important to see your healthcare provider.
What causes insulin resistance?
Scientists still have a lot to discover about how exactly it develops. So far, they’ve identified several genes that make a person more or less likely to develop insulin resistance. Providers also know that gaining weight can worsen it, and losing weight can help improve it. Other factors and conditions can cause varying degrees of the condition.
Acquired causes of insulin resistance
Acquired causes of the condition, meaning you’re not born with the cause, include:
- Excess body fat: Scientists believe obesity is a primary cause of insulin resistance. Excess fat in your belly and around your organs (visceral fat) especially raises your risk.
- Physical inactivity: Movement and exercise make your body more sensitive to insulin. Exercise also builds muscle that can absorb blood glucose. A lack of physical activity can lead to the condition.
- Food choices: A diet of highly processed foods, high in carbohydrates and saturated fats, has been linked to the condition
- Certain medications: Steroids, blood pressure medications, HIV treatments and other medications can cause insulin resistance.
Hormonal disorders that can cause insulin resistance
Issues with certain hormones can affect how well your body uses insulin. Hormonal disorders that can cause insulin resistance include:
- Cushing’s syndrome: This rare condition happens when there’s extra cortisol in your body. Excess cortisol can counteract the effects of insulin, causing the condition.
- Acromegaly: This is a very rare but serious condition that happens when you have high levels of growth hormone (GH). High levels of GH can lead to insulin resistance.
- Hypothyroidism: This means your thyroid is underactive and doesn’t produce enough thyroid hormone. It causes your metabolism to slow down, which can lead to insulin resistance.
Genetic conditions that cause insulin resistance
Certain inherited genetic disorders — conditions you’re born with – can cause the condition for various reasons. These are rare but include Type A insulin resistance syndrome and Donohue syndrome.
Other inherited conditions that can cause it include:
- Myotonic dystrophy: This is a form of muscular dystrophy that affects your muscles, eyes and endocrine system organs.
- Alström syndrome: This condition causes obesity and Type 2 diabetes. It also causes vision and hearing loss, dilated cardiomyopathy and short stature.
- Werner syndrome: A condition that causes accelerated aging (progeria). It affects many aspects of your body, including resistance to the effects of insulin.
- Inherited lipodystrophy: This is a condition in which your body doesn’t use and store fat properly.
Diagnosis and Tests
How is insulin resistance diagnosed?
Insulin resistance is difficult to diagnose because there isn’t routine testing for it. As long as your pancreas is producing enough insulin to overcome the resistance, you won’t have any symptoms.
Your healthcare provider will consider several factors when evaluating you for the condition. These might include your:
- Medical history
- Family history
- Physical exam
- Signs and symptoms
What tests will be done to evaluate insulin resistance?
Your healthcare provider may order the following blood tests to diagnose the condition:
- Glucose test. A fasting plasma glucose (FPG) or a blood glucose test can screen for prediabetes, type 2 diabetes or gestational diabetes.
- A1c test. This test reveals your average blood glucose levels over the past three months.
- Lipid panel. This is a group of tests that measure specific lipids in your blood.
Management and Treatment
How is insulin resistance treated?
Not all factors that contribute to the condition can be treated, such as genetic factors and age. For this reason, lifestyle modifications are the primary treatment for insulin resistance. Lifestyle modifications include:
- Eating nutritious foods. Your healthcare provider may recommend reducing carbohydrates and unhealthy fats. That might mean eating less sugar, red meats and processed starches. Instead, they’ll likely recommend eating more whole foods, like vegetables, fruits and whole grains. For protein, they might suggest more fish and lean poultry.
- Physical activity. Getting regular amounts of moderate-intensity physical activity can help. It helps increase glucose energy usage and improves muscle insulin sensitivity.
- Losing excess weight. In some cases, losing weight can improve insulin resistance. Your healthcare provider can suggest strategies for weight loss.
Over time, these lifestyle modifications can:
- Reduce insulin resistance
- Lower your blood glucose levels
- Decrease blood pressure
- Decrease triglyceride and LDL (“bad”) cholesterol levels
- Raise HDL (“good”) cholesterol levels
Your healthcare provider might refer you to a specialist, like a dietitian or endocrinologist. They’ll work together with you to come up with an individualized treatment plan.
What medications are used to treat insulin resistance?
There are currently no medications that treat the condition specifically. Your healthcare provider may prescribe medications to treat coexisting conditions. Some examples include:
- Blood pressure medication
- Metformin for diabetes or prediabetes
- Statins to lower LDL cholesterol
Can I reverse insulin resistance?
The condition has several causes and contributing factors, and not all causes are reversible. But lifestyle changes can make a difference. Eating nutritious foods, exercising regularly and losing excess weight may decrease your insulin resistance. Talk to your healthcare provider about what you can do to best manage it.
How can diet affect insulin resistance?
What you eat can have a big impact on your blood sugar and insulin levels. The glycemic index (GI) is a tool that can help you determine what foods have the biggest impact on your blood sugar levels.
High-GI foods generally have a lot of carbohydrates and/or sugar. They cause your blood sugar to increase quickly and require a lot of insulin to bring blood sugar back down. You’ll want to avoid high-sugar drinks like regular soda and juices, and avoid eating excess amounts of the following foods:
- White bread
- Potatoes
- Breakfast cereals
- Cakes and cookies
- Fruits such as watermelon and dates
Low-GI foods cause a steadier rise in blood sugar. Your pancreas doesn’t have to work as hard to release insulin. Eating foods that are lower on the glycemic index is generally better for people with insulin resistance:
- Beans and legumes
- Fruits such as apples and berries
- Non-starchy vegetables, such as asparagus, cauliflower and leafy greens
- Nuts
- Dairy, fish and meat
Always talk to your healthcare provider before making extreme changes to your eating patterns.
Outlook / Prognosis
What is the prognosis (outlook) for insulin resistance?
If you have the condition, ask your healthcare provider about what you can expect and how best to manage it.
What you can expect depends on several factors, including:
- The cause of insulin resistance
- The severity of insulin resistance
- How well you and your healthcare provider can manage the condition
People can have mild insulin resistance that never turns into prediabetes or Type 2 diabetes. People can also have insulin resistance that’s reversible or manageable with lifestyle changes.
What are the complications of insulin resistance?
Complications can occur when the condition isn’t managed. Possible complications include:
- Type 2 diabetes
- Metabolic syndrome
- Heart disease
Not everyone who has insulin resistance will have complications. If you’ve been diagnosed with it, it’s important to try to prevent these complications. Be sure to see your healthcare provider regularly and follow your treatment plan.
Prevention
What are the risk factors for developing insulin resistance?
Certain genetic and lifestyle risk factors make it more likely that you’ll develop insulin resistance or prediabetes. Risk factors include:
- Having overweight or obesity, especially excess fat around your belly
- Being age 45 or older
- A first-degree relative (biological parent or sibling) with diabetes
- Being sedentary
- Certain health conditions, such as high blood pressure and high cholesterol levels
- A history of gestational diabetes
- A history of heart disease or stroke
- Having a sleeping disorder, such as sleep apnea
- Smoking
You may have a higher risk of developing it if you are:
- Black
- Hispanic/Latino
- Asian
- Middle Eastern
You can’t change certain risk factors for insulin resistance, such as family history or age. But you can try lowering your chances of developing it by maintaining a healthy weight for you and exercising regularly.
Living With
When should I see my healthcare provider about insulin resistance?
If you’ve been diagnosed with the condition, it’s important to see your healthcare provider regularly. They’ll check to make sure your blood sugar levels are in a healthy range and that your treatment is working.
If you’re experiencing symptoms of high blood sugar or prediabetes, contact your healthcare provider. They can run simple tests to check your blood sugar levels.
If you have a family history of diabetes or insulin resistance, talk to your healthcare provider about your risk of developing it.
What questions should I ask my doctor?
If you receive a diagnosis, it may be helpful to ask your healthcare provider the following questions:
- What’s causing my insulin resistance?
- What’s my risk of developing prediabetes or Type 2 diabetes?
- Is there any medication I can take?
- Should I see a specialist for the condition?
A note from Wockr
Insulin resistance is a complex condition that can affect your health in several ways. It doesn’t have any symptoms until it turns into prediabetes or Type 2 diabetes. The best thing you can do is try to prevent or reverse it by maintaining a healthy weight, exercising regularly and eating nutritious foods. Unfortunately, though, not all causes of the condition are preventable or treatable. If you have any questions about your risk of developing insulin, talk you your healthcare provider. They’re there to help you.