Keratoconjunctivitis
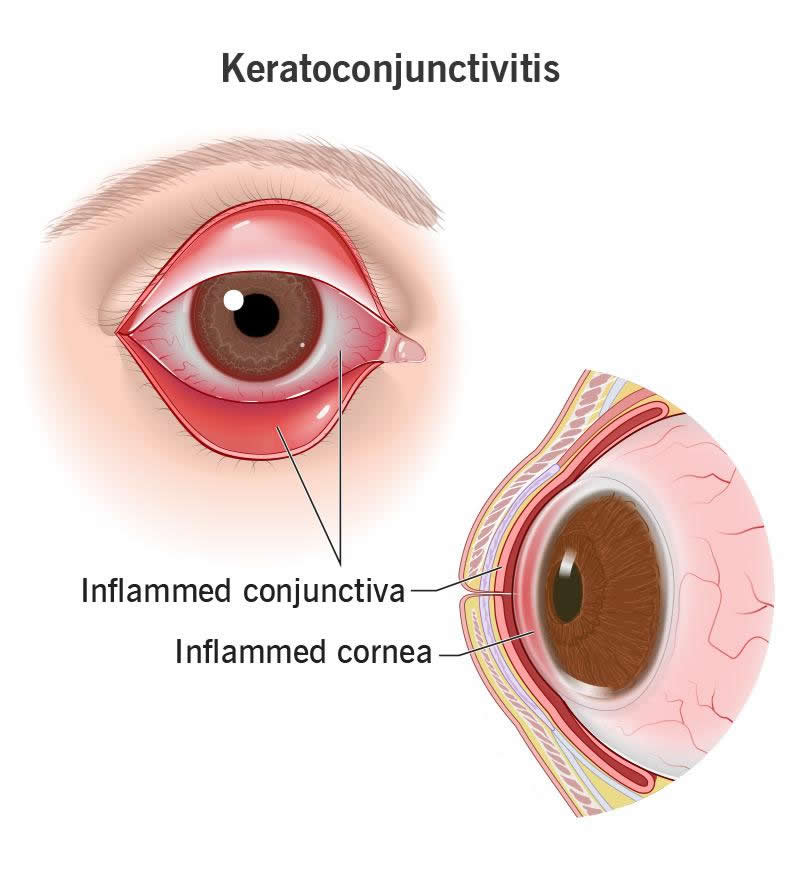
Keratoconjunctivitis is the term for inflammation of your cornea (keratitis) and your conjunctiva (conjunctivitis). These are the clear tissues that cover the surface of your eye. If both are inflamed at the same time, something is seriously irritating your eye. See your healthcare provider right away.
What Is Keratoconjunctivitis?
Keratoconjunctivitis is inflammation of the outer layer of your eyeball. It can happen when an infection, allergen or other irritant gets into your eye. There are also some other, less common causes.
Specifically, keratoconjunctivitis means that two different parts of your outer eyeball are inflamed. Keratitis is inflammation in your cornea. That’s the clear window that covers your iris and pupil (the colored parts of your eye). Conjunctivitis is inflammation in your conjunctiva. That’s the clear film that covers your sclera (the white part of your eye). You may know conjunctivitis by its other name, pink eye.
Keratoconjunctivitis means you have both keratitis and conjunctivitis. So, whatever’s irritating your eye is affecting the whole surface of your eyeball. This might mean it’s more severe than usual.
Types of keratoconjunctivitis
Keratoconjunctivitis has many causes, some of which have their own names. You could consider these subtypes of keratoconjunctivitis. For example:
- Keratoconjunctivitis sicca is a type of dry eye disease (sicca means dry eyes and/or mouth). A problem with your eyes’ tear system causes dryness, which triggers inflammation.
- Vernal keratoconjunctivitis (VKC) is an allergic reaction to airborne allergens. For some people, this seasonal reaction becomes a chronic (long-term) condition.
- Superior limbic keratoconjunctivitis (SLK) is a chronic inflammatory disease. It particularly affects the upper edge of your cornea (superior limbus). The cause is still in debate.
- Epidemic keratoconjunctivitis (EKC) is a highly contagious viral infection caused by adenoviruses. These usually affect your respiratory system, but they can also affect your eyes.
Symptoms and Causes
Symptoms of keratoconjunctivitis
Signs and symptoms of keratoconjunctivitis may include:
- Eye irritation (discomfort, itching or grittiness)
- Swollen eyelids (blepharitis)
- Bumps on your eyes or eyelids
- Red or pink eyes
- Watery eyes
- Eye discharge
- Light sensitivity
- Blurry vision
Keratoconjunctivitis causes
Keratoconjunctivitis is inflammation in your cornea and conjunctiva. Inflammation in any part of your body is a reaction from your immune system. It’s reacting to something that it perceives as a threat.
Many things can trigger keratoconjunctivitis, including eye infections, allergies and autoimmune diseases. Some possible causes include:
- Infectious diseases. Herpetic keratoconjunctivitis, chlamydial keratoconjunctivitis and microsporidial keratoconjunctivitis are caused by different types of infectious diseases.
- Allergic and hypersensitivity reactions. Phlyctenular keratoconjunctivitis, atopic keratoconjunctivitis and vernal keratoconjunctivitis are examples of these reactions.
- Exposure. Dryness and exposure to the elements can injure the surface of your eye. This can happen when you don’t have enough tears (keratoconjunctivitis sicca) or can’t close your eyes.
- Nerve damage. Damage to your fifth cranial nerve can cause neurotrophic keratoconjunctivitis. When your cornea loses sensation, it stops protecting or repairing itself and starts to degrade.
- Autoimmune and autoinflammatory diseases. Chronic immune system diseases can cause ongoing inflammation in different parts of your body, sometimes including your eyes.
- Toxic products. Chemicals, medications or environmental toxins can irritate or injure the surface of your eye. Some people have an immune reaction to the preservatives in their eye drops.
Diagnosis and Tests
How is keratoconjunctivitis diagnosed?
Your eye care provider will start by reviewing your symptoms and medical history. They’ll ask you about your health conditions and any recent illnesses. Your provider may also perform various tests, including:
- An eye exam using slit lamp equipment, with or without a fluorescein eye stain test
- Lab tests on your eye discharge to find the infectious agent
- Lacrimal function tests to determine how well your eyes can create tears
- Imaging tests of your eyes, like ultrasound or MRI
Management and Treatment
Keratoconjunctivitis treatment
Treating keratoconjunctivitis depends on the cause. Some treatments include:
- Artificial tears to lubricate dry eyes, or a lubricating ointment for sleeping
- Warm or cold compresses or lid scrubs to clean your eyes
- Medicated eye drops to treat an infection or allergy (like antibiotics or antihistamines)
For very severe conditions, some people might need eye surgery.
When should I see my healthcare provider about keratoconjunctivitis?
See your healthcare provider if your eyes are red and irritated. See them right away if you have any unusual discharge or vision changes. Some causes of keratoconjunctivitis are more serious than others.
You might want to ask your provider:
- What type of keratoconjunctivitis do I have?
- Is this a short-term or a long-term condition?
- What kind of treatment will I need?
- Will my eyes recover completely?
Outlook / Prognosis
What can I expect if I have keratoconjunctivitis?
Your prognosis depends on the type of keratoconjunctivitis you have. Some types clear up quickly with the right treatment. Others are chronic conditions that may come and go throughout your life. For these types, you may need regular treatment to manage your symptoms.
Treatment for keratoconjunctivitis is usually effective. It can help soothe the inflammation and can often address the underlying cause. But severe keratoconjunctivitis can do permanent damage to your eyes. So, it’s important to get treatment when you need it.
Prevention
How can I reduce my risk of developing keratoconjunctivitis?
You can reduce your risk of keratoconjunctivitis by taking good care of your eyes. For example:
- Wash your hands often and avoid rubbing or touching your eyes
- Use contact lenses safely — always use clean lenses and never sleep in them
- If you have dry eyes, ask your provider to recommend treatments
- Wear sunglasses or other appropriate eye protection when you’re out in the elements
- Avoid known allergens when you can and take allergy medications when you need to
A note from Wockr
If your eyes are itchy and sore, or red where they should be white, contact your eye care specialist for an eye exam. Inflammation can damage your delicate eye tissues, even if it’s a common experience for you. Whether it’s seasonal allergies, an infection or something rarer, it’s important for your provider to isolate the cause so they can determine the best treatment for you.