Osteomalacia
Osteomalacia means “soft bones.” A vitamin D deficiency most often leads to this condition. It causes your bones to soften and weaken. In addition to bone pain, you may notice muscle weakness and stiffness. Treatment for osteomalacia usually includes the use of supplements.
Overview
What is osteomalacia?
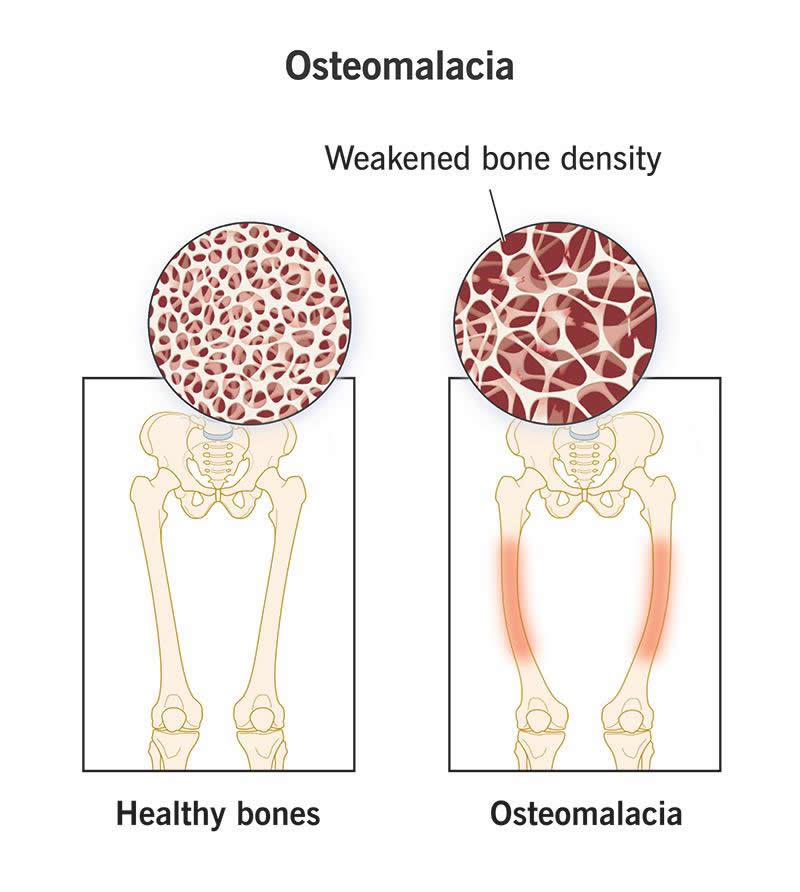
Osteomalacia is a condition in which your bones soften and weaken, causing them to break more easily.
It most often affects adults due to a lack of vitamin D. Your body needs vitamin D to absorb calcium and phosphorous. These minerals help your bones maintain their strength and hardness. Without enough vitamin D, your bones don’t mineralize as they usually would. This leads to bone fragility.
In children, inadequate concentrations of vitamin D may cause a similar condition called rickets.
You may not notice osteomalacia at first. But over time, it can cause bone pain, usually in the lower half of your body. Eventually, you may feel pain all over your body. Simple movements may hurt. Know that you don’t have to live with this pain. Reach out to a healthcare provider. They can help find the cause and offer treatment options.
Symptoms and Causes
What are the symptoms of osteomalacia?
The main symptom of osteomalacia is bone pain. It most commonly affects your hips, pelvis and legs.
Other osteomalacia symptoms may include:
- Bones that break more easily
- Muscle pain, stiffness and weakness, especially after being active
- Difficulty walking or a change in your gait
- Muscle spasms or cramps, especially in your hands and feet
- “Pins-and-needles” feeling (paresthesia) in your arms and legs
- More frequent falls
What is the main cause of osteomalacia?
Osteomalacia develops most commonly due to a vitamin D deficiency. This is often from not getting enough sunlight. But it may also be from not getting enough vitamin D from the foods you eat. Vitamin D is essential for calcium absorption and for maintaining bone health.
Other osteomalacia causes may include:
- A digestive condition that leads to malabsorption
- Kidney failure
- Liver disease
- Antiseizure medications
- Certain rare genetic conditions
What are the risk factors for osteomalacia?
When you’re in sunlight, your skin naturally produces vitamin D. Your skin may not produce enough vitamin D if you:
- Live in a cold, dark climate
- Work inside all day
- Wear clothing that covers most of your skin
- Have darker skin pigmentation
You may not be getting enough vitamin D from the foods you eat if you:
- Don’t consume any milk products
- Follow a vegetarian or vegan diet
- Have a condition that causes malabsorption, like Crohn’s disease or celiac disease
- Have recently had bariatric surgery, like gastric bypass surgery
Other people who have a higher risk of osteomalacia include those who:
- Have obesity
- Are age 65 and older
- Are pregnant or breastfeeding
Diagnosis and Tests
How is osteomalacia diagnosed?
Your healthcare provider will do a physical examination and ask about your family and medical history. They’ll also ask questions about your nutrition and activity level.
Your provider will recommend blood tests to check your levels of vitamin D, calcium and phosphorous. The most significant sign of osteomalacia is low levels of vitamin D. But low calcium or phosphorous levels may also point to osteomalacia.
To confirm a diagnosis, your provider may also check your levels of:
Other tests may include:
- 24-hour urine test to check the amount of calcium in your urine
- X-rays to look for any signs of bone weakening or fractures
- Bone mineral density scan to assess your bone density and monitor for bone loss
- Bone biopsy to see if you have bone softening
Management and Treatment
What is the treatment for osteomalacia?
Osteomalacia treatment includes the use of vitamin D, calcium and/or phosphorus supplements. Your healthcare provider will tell you how much of each of these you need to take. If you have malabsorption issues or recently had bariatric surgery, you may need to take larger doses of vitamin D and calcium.
While supplements should help treat osteomalacia, your symptoms may take several months to improve. Depending on the severity of osteomalacia, you may need to continue taking vitamin D for a long time. If you stop taking it, osteomalacia may return.
People with conditions like liver or kidney failure will need additional treatment and support. Your provider will want to monitor your blood levels regularly. You may need a special form of vitamin D.
Other treatments to relieve or correct osteomalacia symptoms may include:
- Getting enough sunlight exposure
- Eating more foods with vitamin D and calcium
- Wearing braces to reduce or prevent bone irregularities
- Surgery to correct bone deformities (in severe cases)
Outlook / Prognosis
What is the prognosis (outlook) for someone with osteomalacia?
With early diagnosis and treatment (dietary supplements), most people will start to recover from osteomalacia within a few weeks. But it can still take up to six months for your bones to heal and strengthen again.
Prevention
Can I prevent osteomalacia?
Yes, you can usually prevent osteomalacia by:
- Getting enough sunlight
- Getting enough vitamin D and calcium from the foods you eat
Depending on where you live and the time of year, you may be able to get enough vitamin D from sunlight alone. People with lighter skin typically need to expose themselves to 10 to 15 minutes of sunshine two to three times per week. People with darker skin usually need more time in the sun. This must be direct sunlight — not through windows or clothing.
Be careful not to spend too much time in the sun without sunscreen. Too much sun exposure can increase your risk for skin cancer. Ask your healthcare provider about how much time you should spend in the sun.
You won’t be able to get all the vitamin D you need through food alone, but it can help. Some foods naturally contain vitamin D. These include:
- Fatty fish like tuna, salmon, sardines and mackerel
- Rainbow trout
- Red meat
- Beef liver
- Mushrooms
- Egg yolks
- Cod liver oil
Other foods are fortified with vitamin D. Talk to your healthcare provider about which sources are best for you. As with anything, you have to weigh the pros and cons of various foods.
If you’re still not getting enough vitamin D through sunlight and food, your provider may recommend a supplement.
Living With
How do I take care of myself?
As we age, taking care of our bones becomes even more important. To help maintain your bone health:
- Eat an adequate amount of food containing vitamin D and calcium.
- Expose yourself to an adequate amount of sunlight.
- Maintain a healthy weight for you.
- Get regular physical activity.
- Don’tsmoke.
- If you drink beverages containing alcohol, do so in moderation.
When should I see my healthcare provider?
If you have bone pain or any of the other osteomalacia symptoms, reach out to a healthcare provider. They can test your blood levels and determine if this condition is affecting you.
What questions should I ask my healthcare provider?
It may be helpful to ask the following questions:
- Are dietary supplements alone enough to treat osteomalacia?
- What other treatments do you recommend?
- What activities should I avoid while I’m healing?
- What types of exercise can help treat or prevent this condition?
- What else can I do to prevent osteomalacia from affecting me in the future?
A note from Wockr
If you’ve been experiencing bone pain, especially in the lower part of your body, you may have osteomalacia. You can prevent this condition by making sure you get enough vitamin D, whether through sunlight or from the foods you eat. If your symptoms persist, talk to a healthcare provider. They can determine if a vitamin D deficiency is causing your bone pain. And they can help you get on your way to healthier bones.