Tachycardia
Tachycardia is an abnormal heart rhythm with a fast heart rate of more than 100 beats per minute at rest. It can start in the upper or lower chambers of your heart and can range from mild to life-threatening. Treatments include medicines, an ablation procedure and implantable cardioverter defibrillator (ICD) placement.
Overview
What is tachycardia?
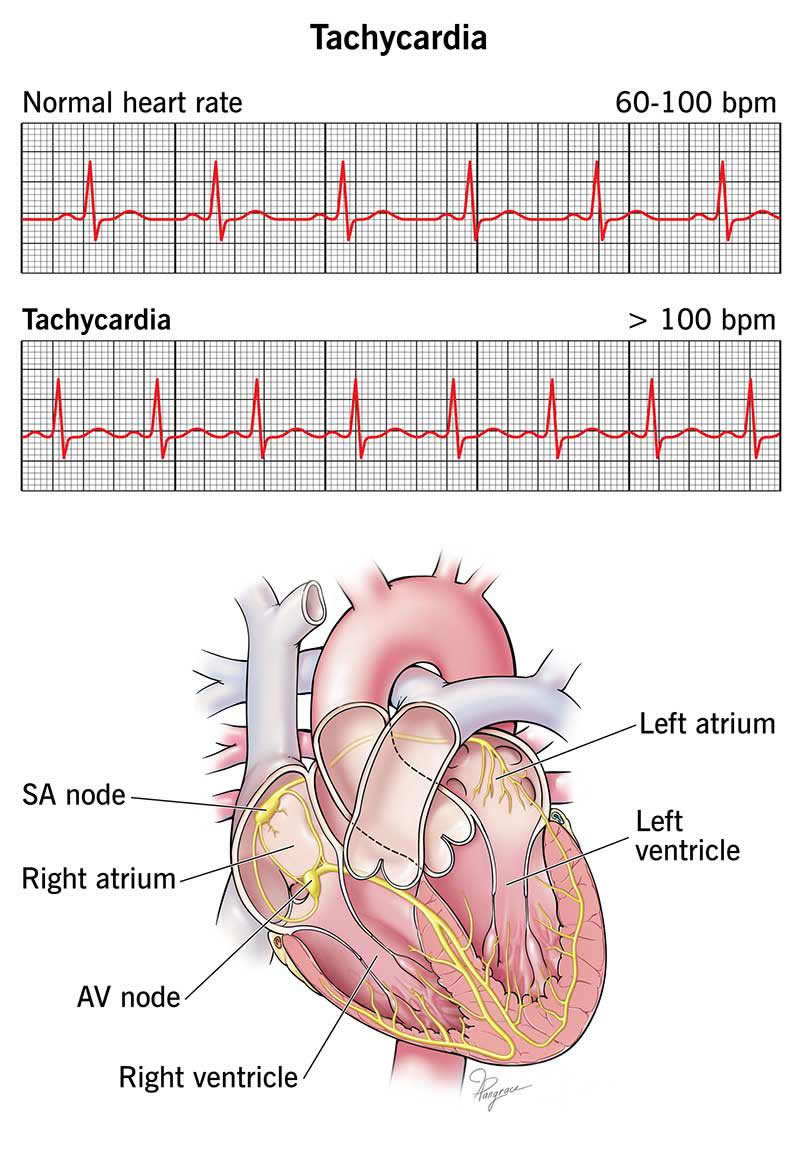
Tachycardia (ta-kih-kar-dee-uh) is a kind of abnormal heart rhythm (arrhythmia). With tachycardia, your heart beats more than 100 times a minute at rest. Your heart beats faster than normal for a few seconds to a few hours. Normally, your heart rate is 60 to 100 beats per minute when you’re not active.
Because your heart beats too often, it doesn’t have the time it needs to fill with blood between beats. This can be dangerous if your heart can’t supply all your cells with the blood and oxygen they need.
Types of tachycardia
Some kinds of tachycardia can come back regularly and can be more serious. Tachycardias can be mild, while others cause issues that are moderately harmful. A healthcare provider can tell you which type of tachycardia you have and how to manage your condition.
Tachycardia can happen in any of your heart’s four chambers. It occurs when you have an issue with electrical signals there.
Types of tachycardia include:
- Supraventricular tachycardias (SVTs), which begin in the atria (upper chambers of your heart). Examples include atrial fibrillation and premature atrial contractions.
- Ventricular tachycardias, which begin in your ventricles, your heart’s lower chambers. Examples include ventricular fibrillation and Torsades de Pointes.
Symptoms and Causes
What are the symptoms?
Some people with tachycardia don’t have symptoms, while others may have mild to severe symptoms. Tachycardia symptoms may include:
- Fast heart rate
- Shortness of breath (dyspnea)
- Chest pain
- Heart palpitations
- Dizziness
- Lightheadedness
- Fainting
- Nausea
- Fatigue
What causes tachycardia?
Your heart normally responds to electrical signals from your heart’s sinoatrial (SA) node. These signals control how often your heart beats. When you’ve had a scare or are very emotional or anxious, or are exercising, your heart may send signals more frequently for a short time. This is called sinus tachycardia and goes away when you calm down or rest.
You may also have a fast heart rate from substance or tobacco use or from too much caffeine or alcohol.
Tachycardia causes include:
- Stress
- Dehydration
- High blood pressure
- Other heart problems, like coronary artery disease
- Low blood sugar
- Pregnancy
- Anemia
What are the risk factors?
Risk factors for tachycardia include:
- Family history of tachycardia
- Obesity
- Diabetes
- Kidney or lung disease
- An untreated thyroid issue
- Certain kinds of medicines, like antiarrhythmics and antidepressants
What are the complications of this condition?
Without treatment, certain types of tachycardia can cause your kidneys, liver or heart to fail. Tachycardia also can lead to:
- Blood clots
- Stroke
- Heart attack
- Cardiomyopathy (weak heart muscle)
- Cardiac arrest
Diagnosis and Tests
How is tachycardia diagnosed?
Your healthcare provider will ask for your medical history and do a physical exam. They may also order tests like:
- Electrocardiogram (EKG)
- Holter monitor or other wearable monitor
- Tilt table test
- Stress test
- Electrophysiology test or EP study
- Echocardiogram
- Blood tests
- Genetic tests
- Cardiac imaging
Management and Treatment
How is tachycardia treated?
Procedures and medications are the main kinds of treatment for tachycardia. Treatments vary depending on the type of tachycardia and what’s causing it. Treatments may include:
- Vagal maneuvers
- Ablation
- Cardioversion
- Implantable cardiac defibrillator (ICD)
- Pacemaker
- Left atrial appendage closure
Medications providers prescribe may include:
- Beta-blockers
- Calcium channel blockers
- Potassium channel blockers
- Sodium channel blockers
- Antiarrhythmic medicines
- Blood thinners or anticoagulants (for atrial fibrillation)
In some situations, you may need CPR.
Outlook / Prognosis
What can I expect if I have tachycardia?
Your experience will depend on which type of tachycardia you have. You may have harmless symptoms, life-threatening symptoms (from ventricular tachycardia or fibrillation) or something in between. Medicines and other treatments can help you manage your high heart rate.
You may need to wear a Holter monitor or do electrophysiology testing to see how well your medicine is working.
How long can tachycardia last?
If you have sinus tachycardia, your symptoms will go away once the fear, anxiety or other emotion that caused it ends. For most other types of tachycardia, you’ll need medication or even a procedure to keep your fast heart rate and other symptoms from coming back.
Tachycardia that puts you in danger doesn’t go away on its own. You’ll need to live a healthy lifestyle and take medicines to manage your condition. You may also need to have a procedure, like an ablation.
Can tachycardia be cured?
Although medications can’t cure tachycardia, they can help you regulate it. Ablation may be a long-term solution to certain types of tachycardia. It may even cure them.
Living With
How do I take care of myself?
You may be able to calm down your tachycardia if your provider teaches you vagal maneuvers.
You can care for yourself in the following ways:
- Manage conditions like high blood pressure and high cholesterol.
- Follow your healthcare provider’s instructions for taking your medicines.
- Drink fewer beverages that contain caffeine and alcohol.
- Stop using tobacco products.
- Aim for a weight that’s healthy for you.
- Eat heart-healthy foods.
- Manage your stress.
When should I see my healthcare provider?
After you get a tachycardia diagnosis, you can expect to have follow-up appointments with your provider. But you should contact them if your medicine isn’t helping you or if you start having new symptoms.
When should I go to the ER?
Get medical help right away if you:
- Have trouble breathing
- Feel your heart pounding
- Have chest pain
- Feel faint or dizzy
You should also get help right away for someone who collapses or is unconscious from ventricular fibrillation. They’ll need CPR to survive until paramedics arrive.
What questions should I ask my healthcare provider?
Questions to ask your provider may include:
- Do I have a dangerous type of tachycardia?
- What kind of treatment do you recommend for me?
- What are your success rates with cardiac ablation?
- Is my family at risk of developing tachycardia?
A note from Wockr
Feeling your heart race can make you stop what you’re doing and wonder what’s going on. Tachycardia symptoms can range from mild to severe, depending on which type of tachycardia you have. For peace of mind, talk to your healthcare provider if you’re having symptoms. They can tell you if you have a reason to be concerned.
Keep taking the medicines your provider prescribed for you, especially heart medicines. Don’t stop taking them without your provider’s approval. And be sure to keep going to all your follow-up appointments.