Vertebral Osteomyelitis
Vertebral osteomyelitis is a rare infection in your spine. It happens when bacteria or fungi infect your vertebrae (spine bones). The infection can start in your spine if the germs get in a wound or surgery site. It can also spread to your spine from somewhere else in your body. You’ll need medication for several weeks to kill the infection.
What is Vertebral Osteomyelitis?
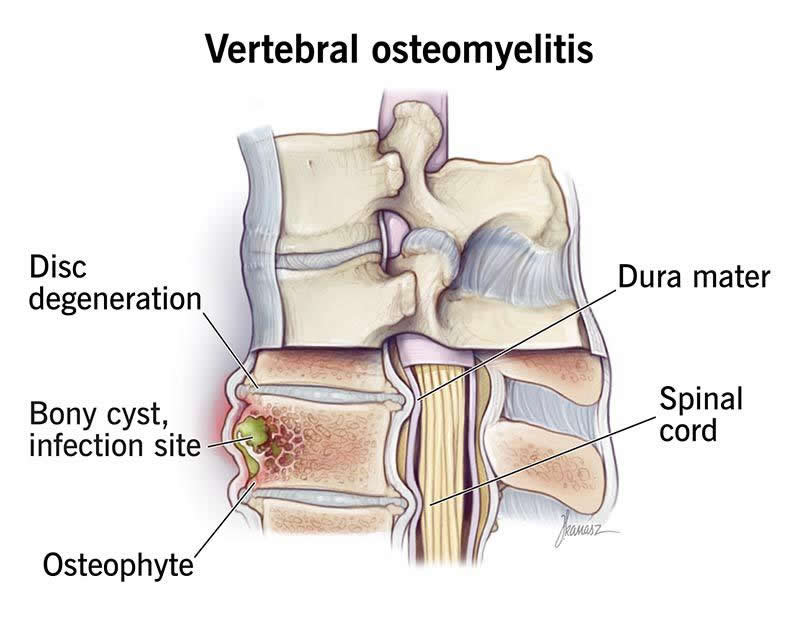
Vertebral osteomyelitis is a rare spine infection. It happens when there’s a bone infection (osteomyelitis) in one of the bones in your spine (vertebrae).
Vertebral osteomyelitis can happen as the result of a spine injury or after surgery. It can also spread to your spine from another place in your body. Other names for this condition include spinal osteomyelitis and spondylodiskitis.
See a healthcare provider right away if you think you might have vertebral osteomyelitis. It can be fatal if it’s not treated.You’ll need medication to treat the infection and other treatments to manage symptoms or complications you experience.
Symptoms and Causes
Symptoms of vertebral osteomyelitis
Symptoms of vertebral osteomyelitis can include:
- Back pain that’s worse when you move and doesn’t get better with at-home treatments
- Numbness and tingling
- Unexpected weight loss
- Weakness
You might feel back pain in one spot (localized) or it might spread (radiate) to other parts of your body. It’s most common to feel pain in your lower back (lumbar spine).
It’s common to have a fever when you have an infection. But you probably won’t if you have vertebral osteomyelitis. Experts estimate that only around 1 in 3 people with vertebral osteomyelitis have a fever they can feel or notice.
Vertebral osteomyelitis causes
Infections that affect your spinal bones cause vertebral osteomyelitis. Bacterial infections are the most common cause, especially staph infections and MRSA. It’s much less common, but some fungal infections can also cause it.
You might have an open wound near your spine after an injury, spine injection or spinal surgery that lets germs in. Or an infection somewhere else in your body can spread to your spine through your bloodstream.
Risk factors
Anyone can get vertebral osteomyelitis, but you may be more likely to if you:
- Live in a nursing home, shared care facility or another place where many people live close together
- Experience a trauma that needs surgery (like repairing a broken bone)
- Have a spine injection
- Have a surgery like a joint replacement
- Have bedsores (pressure injuries)
- Inject recreational drugs or share needles with other people
You might have a higher risk if you have a condition or need treatments that weaken your immune system. Examples include:
- Diabetes
- Sickle cell anemia
- Taking immunosuppressants (like chemotherapy or oral corticosteroids)
- Needing hemodialysis
Complications of vertebral osteomyelitis
Vertebral osteomyelitis complications can include:
- Abscesses.The infection in your spine can cause pockets of pus.
- Necrosis. The infection can kill tissue around your spine if it spreads from your bones into your nerves, skin or spinal cord.
- Osteonecrosis.Severe or untreated infections can cause permanent bone death. This happens if swelling from the infection cuts off blood flow to your vertebrae.
Diagnosis and Tests
How doctors diagnose vertebral osteomyelitis
A healthcare provider will diagnose vertebral myelitis with a physical exam and some tests.
Your provider will examine your back and spine. Tell them when you first noticed pain and other symptoms (especially if certain activities or movements make them worse).
There are a few tests your provider can use to diagnose vertebral osteomyelitis and the infection that caused it. You might need:
Management and Treatment
How is vertebral osteomyelitis treated?
Your healthcare provider will prescribe medication to kill the infection. You’ll need antibiotics if you have a bacterial infection or an antifungal if you have a fungal infection.
Make sure to take your medication for as long as your provider says (even if you start feeling better sooner). If you don’t take the full course, it won’t kill all the bacteria or fungi. This can let the infection come back (recur). Infections that recur are often more severe and have a higher risk of complications.
Your provider might suggest other treatments, including:
- Over-the-counter pain relievers like NSAIDs or acetaminophen to manage pain
- Needle aspiration to drain pus or fluid from your spine
- Surgery to clean out abscesses or repair your spine (this is rare)
- Wearing a back brace to support your spine while you recover
When should I see my healthcare provider?
Vertebral osteomyelitis symptoms can be hard to notice. That’s because back pain is an extremely common issue.
Visit a healthcare provider if you have pain that lasts for more than a few days — especially if rest or other at-home treatments don’t help you feel better. Talk to your provider right away if you notice any changes in your ability to feel or move any part of your body.
Outlook / Prognosis
How serious is vertebral osteomyelitis?
Vertebral osteomyelitis is a serious infection that can be fatal.
With treatment, you may recover from vertebral osteomyelitis in about four to six weeks. However, it might take up to six months to feel fully recovered.
Without treatment, you may develop severe spine damage or blood poisoning (septicemia). Experts estimate that around 1 in 10 people with vertebral osteomyelitis die within a year even though they’ve received a diagnosis and treatment and have gotten better.
A note from Wockr
Thinking about an infection in your spine, like vertebral osteomyelitis, can be scary. But it’s treatable, so don’t hesitate to see a healthcare provider if you think something is wrong. Trust your intuition. You know when pain, weakness or other symptoms aren’t right. The faster a provider can diagnose vertebral osteomyelitis and prescribe medication to treat it, the better.