Heart Valve Disease
Heart valve disease affects the valves that keep your blood flowing in one direction through your heart. Common types of heart valve disease include narrowing (stenosis), backward flow (regurgitation) or stretchy, floppy leaflets that don’t close tightly (prolapse). Treatments include medicines, valve repair or valve replacement.
Overview
What is heart valve disease?
Heart valve disease refers to any of several conditions that prevent one or more of the valves in your heart from working right. Left untreated, heart valve disease may reduce blood flow and cause your heart to work harder. Untreated heart valve disease can become life-threatening.
But there’s hope. In many cases, your healthcare provider can do surgery or a minimally invasive procedure to repair or replace your heart valves. This restores normal function and allows you to return to normal activities.
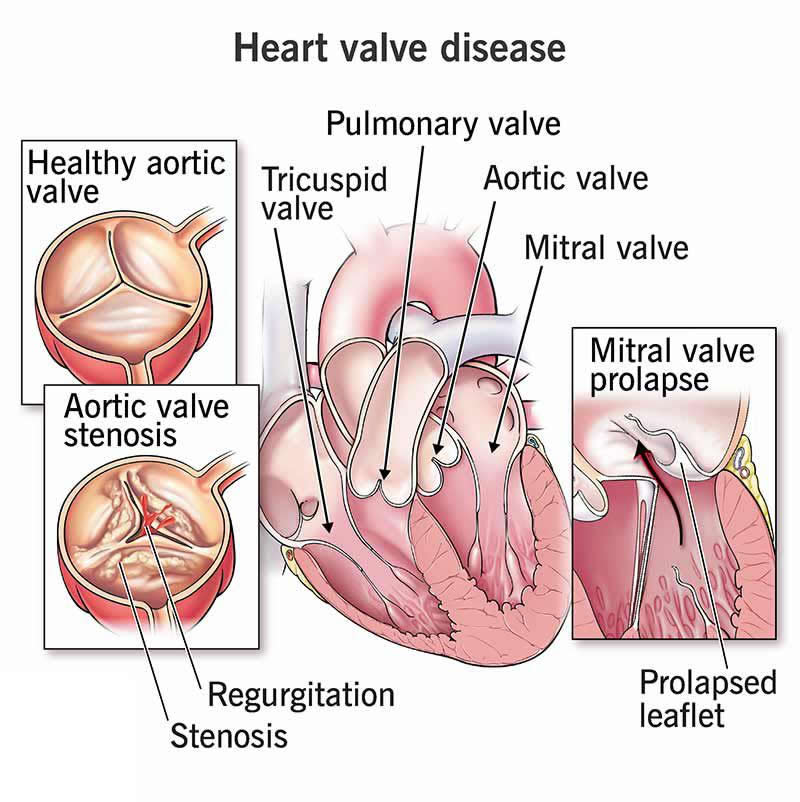
The four valves in your heart make sure blood flows in only one direction through your heart. Your valves consist of small flaps of tissue (called leaflets) that open to allow blood to move forward through your heart during half of your heartbeat. These leaflets close to prevent blood from flowing backward during the other half of your heartbeat.
Your heart’s valves are:
- Mitral (between your left atrium and left ventricle)
- Tricuspid (between your right atrium and right ventricle)
- Aortic (between your left ventricle and aorta)
- Pulmonary (between your right ventricle and pulmonary artery)
Types of heart valve disease
There are different types of heart valve disease: stenosis, regurgitation, prolapse and atresia. They can affect more than one valve.
Stenosis
Tissues forming the valve leaflets become stiffer, narrowing your valve opening and reducing the amount of blood that can flow through it. Mild narrowing may not reduce the overall functioning of your heart. But the valve can become so narrow (stenotic) that it reduces your heart’s function, makes your heart pump harder and puts it under strain. As a result, the rest of your body may not get enough blood flow.
Regurgitation
Also known as insufficiency or "leaky valve," this happens when your leaflets don’t close completely. This lets blood leak backward across your valve. Your heart has to pump harder to make up for this backward flow, and the rest of your body may get less blood flow.
Prolapse
Your mitral valve may not close tightly because the leaflets are extra stretchy. They go back into your left atrium when your heart beats. This is usually harmless, but can lead to regurgitation in some people.
Atresia
Valvular atresia happens when a heart valve forms without an opening before birth. Healthcare providers usually diagnose this very early in infancy.
How common is heart valve disease?
About 2.5% of Americans — many of them older adults — have heart valve disease. Each year, roughly 27,000 people die from heart valve disease in the United States. Mitral valve prolapse is a common heart valve problem.
Symptoms and Causes
What are the first signs of heart valve problems?
Many people with heart valve disease don’t have symptoms. But when the condition worsens over time, your heart beats harder to make up for the reduced blood flow.
Heart valve disease symptoms may include:
- Fatigue (This may be your first symptom.)
- Increasing shortness of breath, especially with physical activity
- Palpitations (skipped beats or a flip-flop feeling in your chest)
- Edema (swelling of your ankles, feet or abdomen)
- Weakness or dizziness
- Quick weight gain
- Chest pain, especially when you exert yourself
What causes heart valve disease?
Common heart valve disease causes include:
- Rheumatic fever from strep throat that wasn’t treated
- Heart attack that damages your heart
- High blood pressure (advanced)
- A congenital (present at birth) issue, like a pulmonary or aortic valve that didn’t develop right
- Decline or calcification of the valve tissue, with loss of function over time
- Thoracic aortic aneurysm (widening of your aorta, which stretches the aortic valve leaflets and can cause leakage)
- Heart failure
- Infection in your heart (infective endocarditis)
- Lupus
- Marfan syndrome
Risk factors
Risk factors that give you a greater chance of getting heart valve disease include:
- Using tobacco products
- Eating foods that aren’t nutritious
- Not getting physical activity
- Having certain conditions like diabetes or high blood pressure
- Getting radiation treatment for cancer
- Having a pacemaker or defibrillator (ICD)
- Being male
- Getting older
What are the complications of heart valve disease?
Untreated valve disease may eventually lead to:
- Heart failure
- Abnormal heart rhythms (arrhythmia)
- Blood clots
- High blood pressure in your pulmonary arteries (pulmonary hypertension)
- Stroke
- Cardiac arrest
Diagnosis and Tests
How is heart valve disease diagnosed?
During a physical examination, a healthcare provider may find these signs of heart valve disease:
- Fluid in your lungs
- An enlarged heart
- A heart murmur, which could mean blood is moving through a narrow or leaky valve
- Swelling in your ankles
Several medical tests can also show heart valve disease. Repeating tests over time can help your provider see the progress of your valve disease and make decisions about your treatment. Valve disease can get worse over time. You may hear a provider describe valve disease with a letter for its stage. Stages start with A and end with D, which is the most severe.
What tests will be done?
Tests for heart valve disease diagnosis include:
- Echocardiogram (heart ultrasound)— A moving image of your heart using sound waves from a handheld wand placed on your chest
- Transesophageal echocardiogram (TEE) — An ultrasound of your heart that uses a probe with a transducer down your esophagus, which sits very close to your heart
- Exercise stress echocardiogram — A test that shows how your valves and heart function after you walk on a treadmill or ride a bike.
- Chest X-ray — A quick X-ray scan of your chest.
- Cardiac catheterization (angiogram) — X-ray movies of your coronary arteries, heart chambers and heart valves.
- Electrocardiogram (EKG or ECG) — Small electrode patches attached to your skin record your heart’s electrical activity.
- Magnetic resonance imaging (MRI) — Radio waves and a magnet work together to create high-quality images of your heart.
Management and Treatment
How is heart valve disease treated?
Heart valve disease treatments depend on the cause and may include:
- Protecting your valve from further damage
- Taking medications
- Having surgery or invasive procedures if necessary
- Seeing your cardiologist (heart doctor) for regular visits
Although you can’t undo damage to a heart valve, you can treat the issue. The decision to prescribe medical treatment, surgical repair or surgical replacement depends on several factors, including:
- The type of valve disease
- The severity of the damage
- Your age
- Your medical history
If you’re pregnant and have heart valve disease, you can get extra rest and/or take certain medicines that are safe for your baby.
If you know about your valve disease before pregnancy, ask your healthcare provider if you should have tests or see a cardiologist before trying to become pregnant. This can help ensure that you get the right treatment before and during pregnancy. If you have a severe valve problem, your provider may recommend valve repair or replacement before pregnancy.
Medications
Although medicines can’t cure heart valve disease, they — and a healthy lifestyle — can help with symptoms and decrease your chance of having a stroke or cardiac arrest. You may be able to stop taking some medications after valve surgery, but you may need to take other medicines for the rest of your life.
Your healthcare provider may prescribe medications to help you with:
- Preventing arrhythmias or blood clots
- Bringing down your blood pressure or cholesterol levels
- Treating heart failure or coronary artery disease
Surgical repair or replacement
Heart valve disease is a problem with the opening or closing of your leaflets, and you may need surgery to repair or replace your valve. Some infants who have congenital (present at birth) valve issues need surgery during childhood.
Usually, the surgeon and cardiologist will know which treatment will be best before surgery day. Other times, the surgeon decides during surgery, when they can see your valve.
Often, providers may combine valve surgery with other procedures (like bypass surgery or surgery to treat atrial fibrillation) to fully treat your heart disease.
Heart valve repair allows your surgeon to fix your faulty valve, often without the use of artificial parts. In some cases, like a narrow mitral valve, your provider may use a balloon on a catheter (valvuloplasty) to widen your valve. They may perform an annuloplasty to fix or reinforce the ring around your valve so it closes better.
The advantages of valve repair are:
- Lower risk of infection
- Decreased need for lifelong blood thinner medication
- Preserved heart muscle strength and function
Surgeons have to replace valves they can’t repair. Replacing your heart valve involves removing your old valve and sewing a new valve to the ring-shaped part of your old one. The new valve could be mechanical or biological (made with tissue from a human, cow or pig). These replacement valves can provide function when repair can’t. But depending on the type of valve you get, you may have to take certain medications to prevent blood clots or get a new valve again in 10 or 15 years.
Depending on the type of valve problem and your other medical conditions, you may be able to have minimally invasive valve repair or replacement.
Complications of treatment
Older people and those whose health isn’t good to begin with have a higher risk of complications from valve replacement surgery.
Complications, which are rarely fatal, may include:
- Infection
- Atrial fibrillation or another type of abnormal heart rhythm
- Bleeding
- Blood clots
- Kidney failure
- Stroke or transient ischemic attack (TIA)
How long does it take to recover from heart valve surgery?
You may be in the hospital for about five to seven days after heart valve surgery. After that, it can take about four to eight weeks to recover. Your provider may recommend cardiac rehab, a carefully monitored program to assist with your recovery.
Outlook / Prognosis
What can I expect if I have heart valve disease?
If you have heart valve disease, you’ll have it for your whole life. But your experience of heart valve disease depends on the valve affected and the severity of the problem.
Some people may have valve disease and never experience any symptoms. Others may have many symptoms and need a valve repair or replacement. Even if your healthcare provider repairs or replaces your valve, you’ll still need to take medicine and possibly have another replacement in 10 or 15 years.
It’s important to follow up regularly with a healthcare provider to monitor the progression of your valve disease over time.
Prevention
How can I reduce my risk of heart valve disease?
Although you can’t change some risk factors, like growing older, there are things you can do that may reduce your risk of heart valve disease. These include:
- Getting treatment quickly for infections
- Being physically active
- Eating heart-healthy foods
- Staying at a weight that’s healthy for you
- Continuing to take medicine for high blood pressure and/or high cholesterol if you have those conditions
- Not using tobacco products
- Not using recreational drugs, especially IV drugs, which increase your risk for heart valve infection
Protecting your valve from further damage
If you have heart valve disease, ask your healthcare provider about the increased risk of getting infective endocarditis. This infection can damage or destroy your heart valves and can be fatal. You’re at risk even if you had surgery to repair or replace your valve. To prevent infective endocarditis:
- Tell your medical and dental providers that you have valve disease
- Call your provider if you have symptoms of an infection
- Take good care of your teeth and gums
- Ask your cardiologist if you should take antibiotics before any dental procedures, major or minor surgeries or invasive tests
Living With
How do I take care of myself?
Keep taking any medicines your healthcare provider prescribed for you and go to all follow-up appointments.
When should I see my healthcare provider?
You’ll need to schedule regular follow-up visits with your cardiologist to make sure your heart valves work as they should. Ask your provider how frequent these visits should be. You may also need to repeat tests, like an echocardiogram.
Contact your provider sooner if your symptoms become more severe or frequent. You should also tell your provider if you have infective endocarditis.
When should I go to the ER?
You should call 911 or your local emergency number if you have these symptoms after heart valve surgery:
- Syncope (fainting)
- Fever or chills
- Upset stomach or diarrhea
- Chest pain
- Heart rate of more than 150 beats a minute
- Severe headache, arm or leg weakness, or numbness without warning
- Shortness of breath that doesn’t get better with rest
- Bright red blood in what you cough up
- Dark black stool or bright red blood in your stool
What questions should I ask my healthcare provider?
Questions to consider asking your provider include:
- Would lifestyle changes help me?
- What kinds of physical activity are safe for me to do?
- How soon after surgery can I be physically active?
A note from Wockr
It can be a relief to know that the fatigue you’ve been feeling isn’t part of aging. The good news about a heart valve issue is that you can manage it with medications and/or surgery. Your healthcare provider can talk with you about the best option for you. Regardless of what your provider does, you can help yourself feel better by being more physically active, eating heart-healthy foods and avoiding tobacco products. Be sure to keep taking any prescribed medicines and go to all of your follow-up appointments.